HIV is one of the diseases that has significantly impacted humanity for a long time. Although antiretroviral therapy (ART), a key form of HIV medication, helps individuals with HIV live longer and reduces the risk of transmission, completely eradicating the virus from the body remains a major challenge. People living with HIV still rely on ART and other HIV medications for lifelong treatment, as the virus can hide within immune cells.
Recently, Immunocore, a company based in the United Kingdom, has developed a new technology called the Bispecific T Cell Receptor (TCR), which has the potential to directly eliminate HIV from the body. This innovation not only brings new hope to individuals living with HIV worldwide but could also transform the treatment of other infectious diseases in the future. This article explores this significant advancement in HIV medication and treatment, and its potential impact on the medical field and global society.
What is the current state of HIV Medication ?
Currently, HIV treatment focuses on the use of Antiretroviral Therapy (ART), a highly effective combination of medications that suppress the replication of HIV in the body. ART works by disrupting various processes of the virus, such as its replication or entry into the body’s cells, to prevent the virus from multiplying. While it cannot completely eliminate the virus, ART can control the viral load in the bloodstream to extremely low levels, making it undetectable, a condition referred to as Undetectable Viral Load.

Effects of HIV Treatment with Antiretroviral Therapy (ART)
The use of ART has shown impressive results in several areas:
- Improved Health for Individuals with HIV: People living with HIV can lead long, healthy lives comparable to those without the virus if they take their medication consistently and have regular medical follow-ups.
- Reduced Risk of Transmission: When the viral load in the body decreases to an undetectable level, the risk of transmitting HIV through sexual contact is significantly reduced. This represents a crucial step in controlling the spread of HIV.
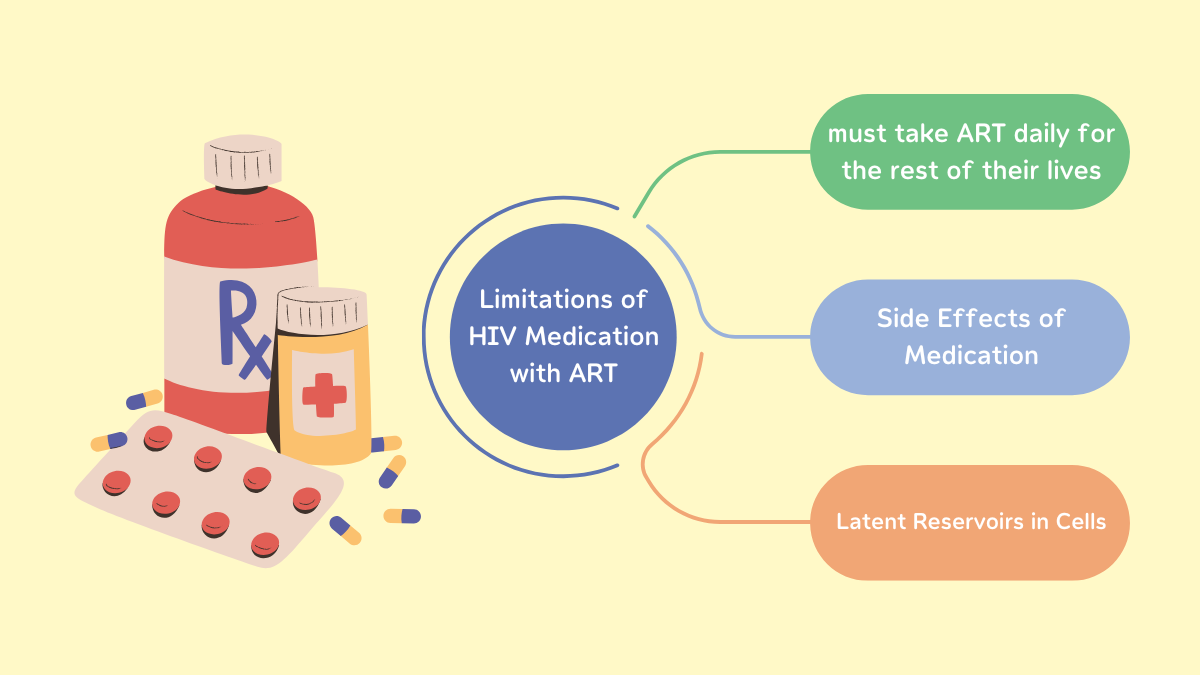
Limitations of HIV Medication with ART
Although ART significantly improves the quality of life for people living with HIV, there are still important limitations to this approach:
- Lifelong Dependence on Medication
- Individuals with HIV must take ART daily for the rest of their lives. Stopping the medication can cause a rapid increase in the viral load (viral rebound), leading to a weakened immune system and a higher risk of complications or transmission.
- Side Effects of Medication
- While newer ART drugs have fewer side effects compared to earlier treatments, some individuals still experience issues such as nausea, fatigue, or long-term problems with the liver and kidneys.
- Latent Reservoirs in Cells
- HIV has the unique ability to hide within CD4+ T cells, a type of white blood cell critical to the immune system. These cells act as reservoirs where the virus remains in a dormant state. ART cannot reach or eliminate the virus in these latent reservoirs.
As long as HIV hides in these cells, the immune system cannot detect or destroy the infected cells. This is the primary reason why current HIV treatments cannot achieve a complete cure.
New Technology: Bispecific T Cell Receptor (TCR)
Bispecific T Cell Receptor (TCR) is an innovative development by Immunocore, specifically designed to target and eliminate HIV-infected cells. This groundbreaking technology holds great promise in addressing the limitations of antiretroviral therapy (ART), which cannot remove latent viruses hidden in cells.
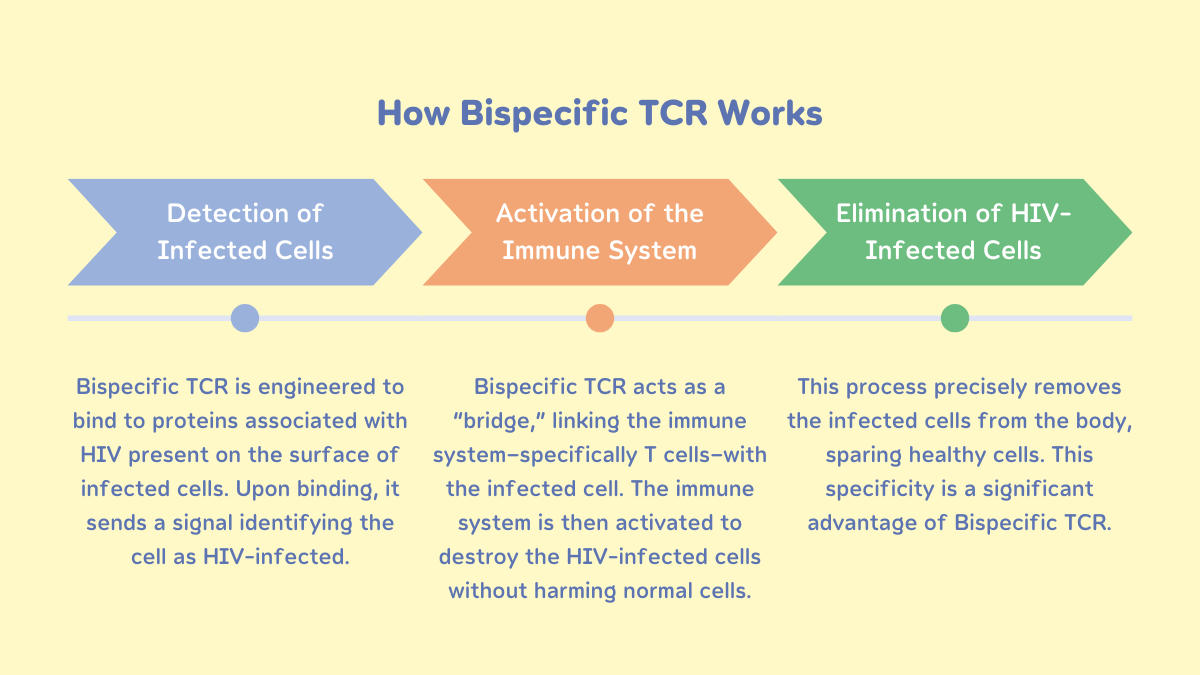
How Bispecific TCR Works
The technology utilizes a specially designed protein to detect specific proteins expressed on the surface of HIV-infected cells. The process involves three key steps:
| 1. Detection of Infected Cells | Bispecific TCR is engineered to bind to proteins associated with HIV present on the surface of infected cells. | Upon binding, it sends a signal identifying the cell as HIV-infected. |
| 2. Activation of the Immune System | Once the infected cell is identified, Bispecific TCR acts as a “bridge,” linking the immune system—specifically T cells—with the infected cell. | The immune system is then activated to destroy the HIV-infected cells without harming normal cells. |
| 3. Elimination of HIV-Infected Cells | This process precisely removes the infected cells from the body, sparing healthy cells. This specificity is a significant advantage of Bispecific TCR. | |
Advantages of Bispecific TCR
- High Precision: Bispecific TCR is designed to specifically target HIV-associated proteins, reducing the risk of damaging healthy cells.
- Natural Immune System Activation: Unlike treatments that rely on chemotherapy or other drugs, this technology leverages the body’s immune system to eliminate the virus, making it a safer treatment option.
- Reduced Risk of Drug Resistance: By targeting and eliminating the virus directly within infected cells, this approach minimizes the likelihood of the virus developing drug resistance, which is a common challenge for long-term ART users.
Preliminary Results of Bispecific TCR
The Phase 1 trials, conducted on a small group of participants, have demonstrated the potential of this innovative technology:
◀ Effective Detection of Infected Cells
Bispecific TCR successfully
identified and eliminated
HIV-infected cells
with high efficiency.
◀ High Safety Profile
The technology caused no harm
to uninfected cells, addressing
a major concern associated
with other treatment approaches.
◀ Potential for Broader Application
Although still in its early stages,
the promising results have sparked
optimism for future trials in larger
and more diverse groups.
Other Approaches in HIV Treatment: Diverse Advancements
While Bispecific TCR technology offers an exciting new hope, researchers continue to develop additional methods to enhance options and improve the chances of completely eradicating HIV. These approaches focus on both eliminating the virus and strengthening the immune system of individuals living with HIV.

1. Broadly Neutralizing Antibodies (bNAbs)
Broadly Neutralizing Antibodies (bNAbs) are a specialized type of antibody that can bind to and neutralize various strains of HIV. They play a crucial role in boosting the immune system’s ability to combat the virus.
How bNAbs Work:
- Binding to Key Proteins on the Virus: bNAbs can attach to specific proteins on the surface of HIV, such as gp120 and gp41, which the virus uses to enter cells.
- Neutralizing Multiple HIV Strains: One of the standout features of bNAbs is their ability to tackle a wide variety of HIV strains, making them effective across diverse patient populations.
- Enhancing Immune System Response: bNAbs promote the activity of T cells and other immune cells, enabling a more robust and effective response against the virus.
Advancements in bNAbs Research
Research on using bNAbs as part of HIV treatment is still in the development phase. However, early studies have shown that:
- Injecting bNAbs in combination with antiretroviral therapy (ART) can significantly reduce viral load in the bloodstream.
- bNAbs may help decrease the dependence on lifelong ART by offering a complementary approach to managing the virus.
These advancements highlight the potential of bNAbs to become an integral part of future HIV treatment strategies, providing patients with more effective and lasting solutions.
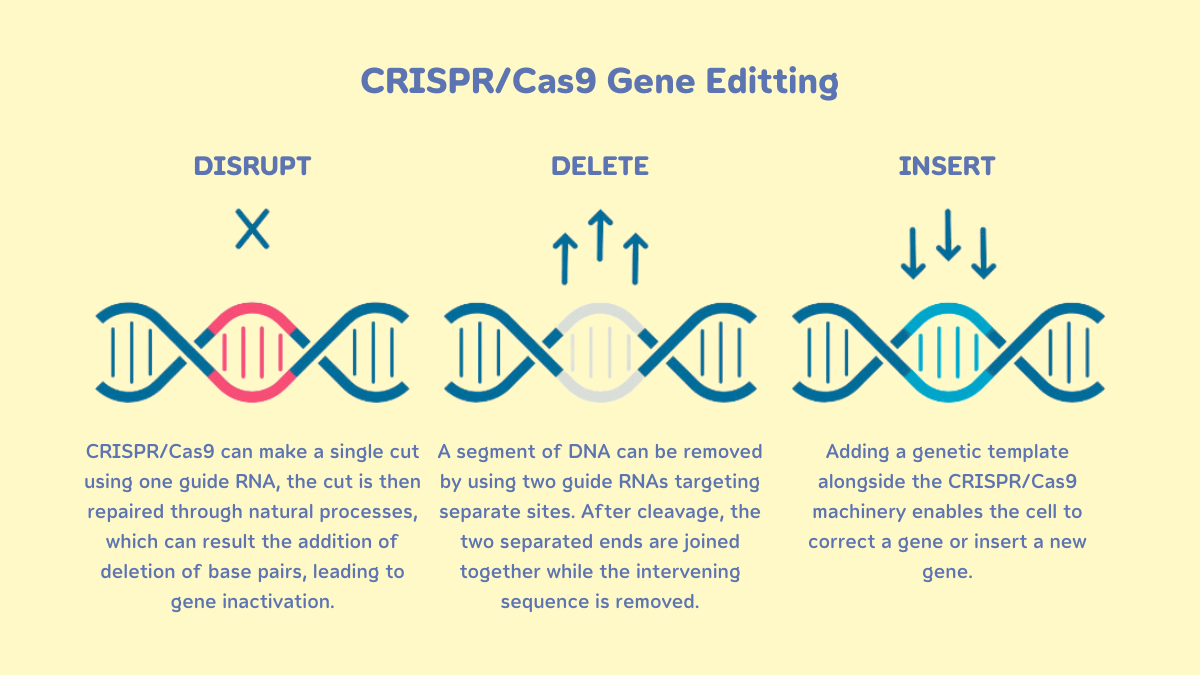
2. Gene Editing: A Revolutionary Approach to HIV Treatment
Gene Editing is a highly promising technology in the development of HIV treatment, particularly through the use of CRISPR-Cas9, a precise and powerful gene-editing tool.
How CRISPR Works in HIV Treatment
- Editing Immune Cells
- Researchers use CRISPR to modify the genes of CD4+ T cells, the primary target of HIV.
- These edits enhance the immune cells’ resistance to HIV infection, making them less vulnerable to the virus.
- Eliminating Embedded Virus
- CRISPR can locate and cut out the genes of the virus embedded in the DNA of infected cells.
- This method helps reduce the latent reservoir, where HIV remains dormant, and lowers the chance of the virus reactivating.
Advantages of Gene Editing
- High Precision: CRISPR’s accuracy allows for targeted gene modifications, reducing unwanted side effects.
- Reduced Dependence on Medication: Successfully editing immune cells may eliminate the need for lifelong antiretroviral therapy (ART), offering patients a more sustainable treatment option.
“The use of Gene Editing in HIV treatment is still in the experimental phase.
The key challenges lie in assessing its long-term safety and implementing it on a broader scale.”
The Importance of Supporting Research for an HIV Medication
Developing a cure for HIV requires immense collaboration and resources. It is not solely about medical innovation but also involves collective efforts from governments, private sectors, and communities at all levels.
1. Significant Resource Investment
HIV research and development demand:
- Funding: Clinical trials, innovative technologies like Bispecific TCR and Gene Editing, and long-term impact studies require substantial financial investment.
- Skilled Professionals: Scientists, doctors, and specialized researchers are crucial for advancing HIV treatment. Training and retaining such talent are essential for sustained progress.

2. Support from Governments and International Organizations
- Role of Governments
- Allocating budgets and creating policies that foster research, such as dedicated funds for infectious diseases and tax incentives for companies investing in health research.
- Promoting international collaboration through the exchange of medical knowledge and data to improve treatment development.
- Role of International Organizations
- Organizations like UNAIDS and WHO play vital roles in coordinating global efforts and mobilizing resources to support research in underprivileged areas.
- Their efforts help reduce disparities and enable individuals in developing countries to access necessary treatments.
3. Reducing Stigma and Improving Access to HIV Medication
Reducing Stigma
Many individuals with HIV face social stigma, discouraging them from seeking testing and treatment. Education and community awareness are essential to combat this issue and ensure patients receive proper care.
Improving Access for Marginalized Groups
- In many regions, particularly in developing countries, access to antiretroviral therapy (ART) and healthcare remains a challenge due to:
- High treatment costs.
- Lack of adequate public health infrastructure.
- Shortages of medical personnel.
- Support from global organizations and increased funding can ensure equitable access to treatment for all affected individuals.
4. The Broader Impact of HIV Research
Support for HIV research not only advances treatment for the disease itself but also drives progress in other medical fields, such as:
- Vaccine Development: Insights from HIV vaccine research can contribute to vaccines for other infectious diseases.
- Gene Editing Technology: Studies on HIV-related gene editing open avenues for treating genetic disorders and cancer.
FAQ About HIV Medication
Answer: Yes, HIV can be managed with antiretroviral therapy (ART). These medications control the virus, prevent it from replicating extensively in the body, and help individuals with HIV maintain strong health and avoid illness.
Answer: Yes! ART is essential to suppress the virus. Stopping medication can cause the virus to increase and may lead to transmission. Consistent medication is vital for maintaining good health.
Answer: Take your medication at the same time every day without skipping doses. Consult your doctor if you experience side effects like nausea, headaches, or fatigue.
Answer: HIV is the virus that causes the infection. AIDS is the advanced stage of untreated HIV, where the immune system becomes severely weakened, leading to life-threatening complications.
Answer: Yes! If the virus is suppressed to undetectable levels in the blood (Undetectable Viral Load), it cannot be transmitted through sexual contact (U=U). Learn more at www.uuandme.org
Related Articles
- HIV and Mental Health : Understanding the Connection and Coping Strategies
- Positive Living: Thriving with HIV
Conclusion
The search for a definitive cure for HIV remains one of the greatest challenges in modern medicine. However, advancements in technology, such as the Bispecific T Cell Receptor (TCR), research into antibodies, Gene Editing, and vaccines, are providing new hope for people living with HIV worldwide. These developments not only enhance the potential for HIV treatment but also push the boundaries of medical science in addressing other complex diseases.
Achieving complete eradication of HIV requires support from all sectors. Investment in resources, fostering international collaboration, and reducing the stigma surrounding HIV are crucial factors in driving scientific progress and ensuring equitable access to treatment. With the dedication and cooperation of scientists, organizations, and society, we may soon reach a day when HIV is no longer a global threat, marking a transformative milestone in human history.
Reference:
ดร.อนันต์ เผยบริษัทดังในอังกฤษ ค้นพบวิธีรักษาผู้ติดเชื้อ HIV ให้หายขาด
- pptvhd36.com/health/news/6381
เผยข่าวดีสำหรับผู้ติดเชื้อ HIV บริษัทดังในอังกฤษ ค้นพบวิธีรักษาให้หายขาดหลังต่อสู้มากว่า 40 ปี
- matichon.co.th/local/quality-life/news_4990843
Immunocore announces strategic priorities at 43rd Annual J.P. Morgan Healthcare Conference
- manilatimes.net/2025/01/10/tmt-newswire/globenewswire/immunocore-announces-strategic-priorities-at-43rd-annual-jp-morgan-healthcare-conference/2036702
Novel vaccine concept generates immune responses that could produce multiple types of HIV neutralizing antibodies
- medicalxpress.com/news/2024-05-vaccine-concept-generates-immune-responses.html

