-
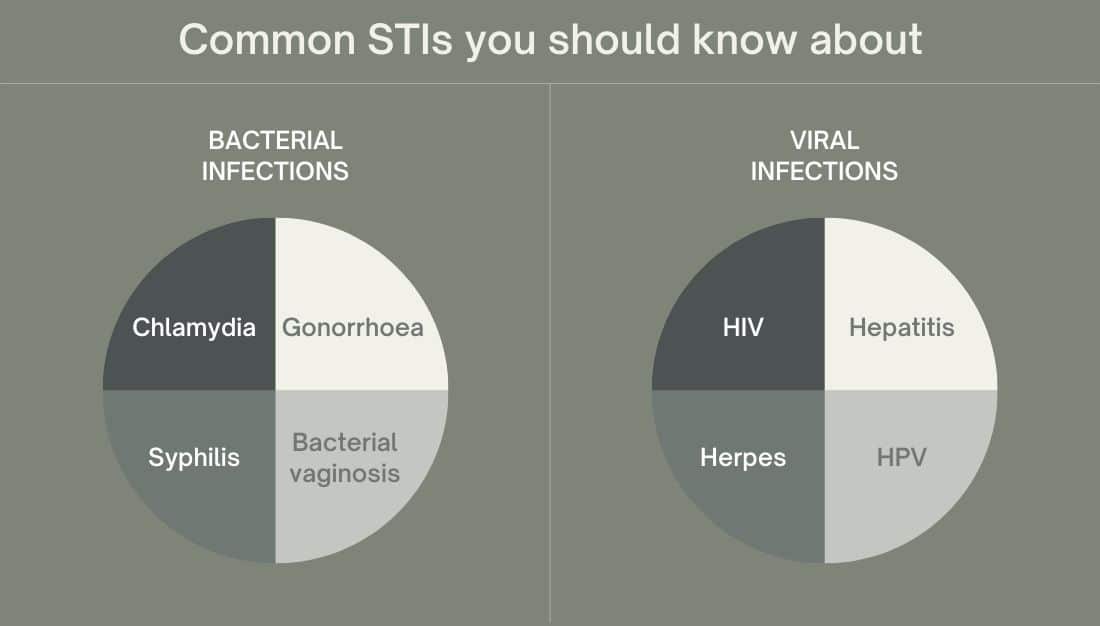
More than 30 different bacteria, viruses and parasites are known to be transmitted through sexual contact. Eight of these pathogens are linked to the greatest incidence of sexually transmitted disease. Of these, 4 are currently curable: syphilis, gonorrhoea, chlamydia and trichomoniasis. The other 4 are viral infections which are incurable: hepatitis B, herpes simplex virus (HSV or herpes), HIV and human papillomavirus (HPV).
What is a sexually transmitted infection (STI)?
A sexually transmitted infection (STI) is caused by an organism (bacteria, virus, or parasite) that can be passed from one person to another during sex or intimate contact.
Most STIs are passed (or transmitted) between sexual partners through unprotected oral, vaginal (frontal) or anal sex. Some STIs are passed by skin-to-skin contact. Using condoms and other barriers for vaginal (frontal), oral and anal sex is a good way to lower the chances of passing many STIs.
An infection is when a bacteria, virus, or parasite enters and grows in or on your body. Some STIs can be cured and some STIs cannot be cured. For those STIs that cannot be cured, there are medicines to manage the symptoms.
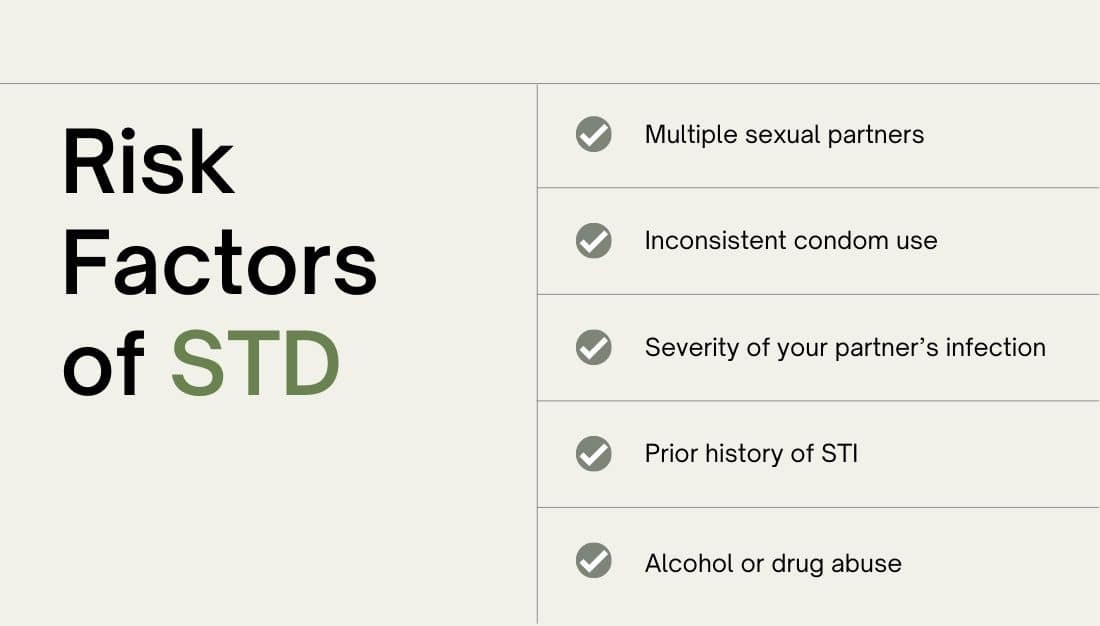
Who is at risk for an STI?
- you don’t use condoms during sex or dental dams (a thin latex square held over the vaginal or anal area during oral sex)
- you have changed sex partners or had more than one sex partner in the last 12 months
- you or your partner share injecting equipment such as a syringes and needles
- you or your sex partner has another STI.
How do you get STIs?
- Having unprotected (without a condom) vaginal, oral, or anal sex with someone who has an STI. It can be difficult to tell if someone has an STI. STIs can be spread even if there are no signs or symptoms.
- During genital touching. It is possible to get some STIs, such as syphilis and herpes, without having sex.
- Through sexual contact between women who have sex only with other women
- From a pregnant or breastfeeding woman to her baby
What are the symptoms of STIs?
When you get an STI you may not have any obvious symptoms. You can feel perfectly okay and not realise you have an infection. But even if you don’t notice any signs the STI could still be making you sick.
Some STI symptoms could include:
- unusual discharge from your vagina or penis
- difficulty or pain when you urinate and have sex
- blisters, warts, lumps, bumps or sores on your genitals
- rash, cracked skin, itchy or irritated skin on or around your genital region.
How do I know if I have an STI?
If you notice any of the above symptoms, or if you had sex without a condom or a dental dam, you and your sex partner(s) should see a doctor for an STI check. Depending on your particular circumstances, this may involve a urine sample, swab and/or blood test.
The earlier you are diagnosed with an STI, the easier it is to treat which also reduces the chances of you developing further health complications.
Diagnosis of STIs
Ask your doctor or nurse about getting tested for STIs. Your doctor or nurse can tell you what test(s) you may need and how they are done. Testing for STIs is also called STI screening.
How do I get tested for STIs?
- Laboratory tests. can identify the cause and detect coinfections you might also have.
- Blood tests. Blood tests can confirm the diagnosis of HIV or later stages of syphilis or test for an STI.
- Urine samples. Some STIs can be confirmed with a urine sample. Fluid or tissue sample.
- Fluid or tissue sample. Your doctor or nurse uses a cotton swab to take fluid or discharge from an infected place on your body. The fluid is looked at under a microscope or sent to a lab for testing.
- Pelvic and physical exam. Your doctor looks for signs of infection, such as warts, rashes, or discharge.
Do I need to get tested for STIs?
If you are sexually active, talk to your doctor or nurse about STI testing. Which tests you will need and how often you need to get them will depend on you and your partner’s sexual history.
You may feel embarrassed or that your sex life is too personal to share with your doctor or nurse. But being open and honest is the only way your doctor can help take care of you. Find out what screening tests you may need. Then talk to your doctor or nurse about what tests make sense for you.
How are STIs treated?
Many STIs are successfully treated with antibiotics. Others can be managed with medication.
Treatment of STIs
STIs caused by bacteria are generally easier to treat. Viral infections can be managed but not always cured.
If you are pregnant and have an STI, getting treatment right away can prevent or reduce the risk of your baby becoming infected.
Treatment for STIs usually consists of one of the following, depending on the infection:
Antibiotics. Antibiotics
often in a single dose, can cure many sexually transmitted bacterial and parasitic infections, including gonorrhea, syphilis, chlamydia and trichomoniasis. Typically, you’ll be treated for gonorrhea and chlamydia at the same time because the two infections often appear together.
Once you start antibiotic treatment, it’s necessary to finish the prescription. If you don’t think you’ll be able to take medication as prescribed, tell your doctor. A shorter, simpler course of treatment may be available.
In addition, it’s important to abstain from sex until seven days after you’ve completed antibiotic treatment and any sores have healed. Experts also suggest women be retested in about three months because there’s a high chance of reinfection.
Antiviral drugs.
If you have herpes or HIV, you’ll be prescribed an antiviral drug. You’ll have fewer herpes recurrences if you take daily suppressive therapy with a prescription antiviral drug. However, it’s still possible to give your partner herpes.
Antiviral drugs can keep HIV infection in check for many years. But you will still carry the virus and can still transmit it, though the risk is lower.
The sooner you start HIV treatment, the more effective it is. If you take your medications exactly as directed, it’s possible to reduce the viral load in the blood so that it can hardly be detected.
If you’ve had an STI, ask your doctor how long after treatment you need to be retested. Getting retested will ensure that the treatment worked and that you haven’t been reinfected.
If I have an Sexually transmitted infections, does my partner have it too?
Maybe. If the tests show that you have an STI, your doctor might want your partner to come in for testing. Or the doctor may give you a medicine to take home for your partner.
The STI may have spread to you or your partner from a former sex partner. This is why it is important to get tested after each new sex partner.
How can I prevent an Sexually transmitted infections?
The best way to prevent an STI is to not have vaginal, oral, or anal sex.
If you do have sex, lower your risk of getting an STI with the following steps:
- Get vaccinated. There are vaccines to protect against HPV and hepatitis B.
- Use condoms. Condoms are the best way to prevent STIs when you have sex. Because a man does not need to ejaculate (come) to give or get some STIs, make sure to put the condom on before the penis touches the vagina, mouth, or anus. Other methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from STIs.
- Get tested. Be sure you and your partner are tested for STIs. Talk to each other about the test results before you have sex.
- Be monogamous. Having sex with just one partner can lower your risk for STIs. After being tested for STIs, be faithful to each other. That means that you have sex only with each other and no one else.
- Limit your number of sex partners. Your risk of getting STIs goes up with the number of partners you have.
- Do not douche. Douching removes some of the normal bacteria in the vagina that protects you from infection. This may increase your risk of getting STIs.
- Do not abuse alcohol or drugs. Drinking too much alcohol or using drugs increases risky behavior and may put you at risk of sexual assault and possible exposure to STIs.
- The steps work best when used together. No single step can protect you from every single type of STI.
Common STIs include:
- Gonorrhoea caused by the bacteria Neisseria gonorrhoeae. This infection can occur in the penis or external genitals, vagina or internal genitals, anus, and eye. The bacteria can also be found in body fluids such as semen, pre-ejaculate, vaginal fluids, and anal fluids.
- Chlamydia caused by the bacteria Chlamydia trachomatis. Infections can occur in the penis or external genitals, vagina or internal genitals, anus, throat, and eye. The bacteria can also be found in body fluids such as semen, pre-ejaculate, vaginal fluids, and anal fluids.
- Genital herpes caused by the herpes simplex virus (HSV). HSV Type I is more common on the mouth (cold sores) and HSV Type II on the genitals, but both viruses can infect the mouth and genital area.
- Genital warts they are small lumps on the genitals which you can see or feel. They are usually painless. They are caused by the human papilloma virus (HPV).
- Syphilis caused by the bacteria Treponema pallidum. Syphilis infection occurs in stages: primary, secondary, early latent and late latent. Each stage has different symptoms associated with it.
Anoter STIs
Hepatitis B
- is a preventable liver disease caused by the hepatitis B virus (HBV). Hepatitis B ranges in severity from a mild illness, lasting a few weeks (acute), to a serious long-term (chronic) illness that can lead to liver disease or liver cancer.
Human Immunodeficiency Virus (HIV)
- is a virus that targets the body’s immune system. It is passed through blood and body fluids such as semen, pre-ejaculate, vaginal fluids, anal fluids, and breast/chest milk. HIV can be managed with antiviral medications. If left untreated, HIV can cause AIDS (acquired immune deficiency syndrome). AIDS occurs when the body’s immune system is weakened and is unable to fight off infections and illnesses effectively.
Bacterial vaginosis (BV)
- is an imbalance of the naturally-occurring. Healthy bacteria found in the vagina or internal genitals. When conditions change, certain bacteria can increase and create symptoms. Infections can only occur in a vagina/internal genitals. BV can be treated with antibiotics.
Cystitis
- is an inflammation (swelling) of the bladder, usually caused by an infection. It affects women more than men, and can occur at any age.
Giardia infection (giardiasis)
- is a bowel (gut) infection caused by a tiny parasite called Giardia lamblia, also known as Giardia intestinalis. The parasite is a single-celled organism that can attach itself in large numbers to the wall of your bowel and interferes with your body’s natural absorption of nutrients.
Human papillomavirus (HPV)
- is highly contagious and can cause a variety of cancers and genital warts.In most of us the infection is invisible, harmless and goes away after a few months without causing any problems. There are over 100 different types of HPV, which infect different parts of the body. Around 50 types can infect the genitals, including the cervix (the neck of the uterus).
Lymphogranuloma venereum (LGV)
- is a sexually transmitted infection (STI) caused by a strain of chlamydia bacteria. Infections usually occur in the lymphatic system in the genital area. The bacteria can also be found in body fluids such as semen, pre-ejaculate, vaginal fluids, and anal fluids.
Molluscum contagiosum
- is a skin infection caused by a pox virus and can occur anywhere on the skin. It is very common in children. It is less common in adults and is usually spread through sexual contact. In this case, infections usually occur on the stomach, genital area, buttocks, and thighs.
Pelvic inflammatory disease (PID)
- is an infection of the upper genital tract, including the uterus, fallopian tubes, and ovaries. It happens when infections travel up from the vagina or internal genitals through the cervix.
Pubic lice
- (often called “crabs”) are parasites that live on body hair, usually in the genital area. Occasionally they are found on hair on the legs, armpits, mustache, beard, eyebrows, or eyelashes. Pubic lice can be treated with a special shampoo.
Scabies
- is a skin infection caused by the parasite Sarcoptes scabiei. Scabies usually occurs on the hands, armpits, wrists, nipples, waist, abdomen, genitals, and thighs. Scabies can be treated with lotions or creams.
Trichomoniasis
- is a sexually transmitted infection (STI) caused by the parasite Trichomonas vaginalis. Infections can occur in a penis or external genitals, and a vagina or internal genitals. The parasite can also be found in body fluids such as semen, pre-ejaculate, and vaginal fluids.
References
Sexually transmitted infections (STIs)
- who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
Sexually transmitted infections
- womenshealth.gov/a-z-topics/sexually-transmitted-infections
Sexually transmitted infections (STIs)
- healthywa.wa.gov.au/Articles/A_E/About-sexually-transmitted-infections-STIs
Sexually transmitted diseases (STDs)
- mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/diagnosis-treatment/drc-20351246