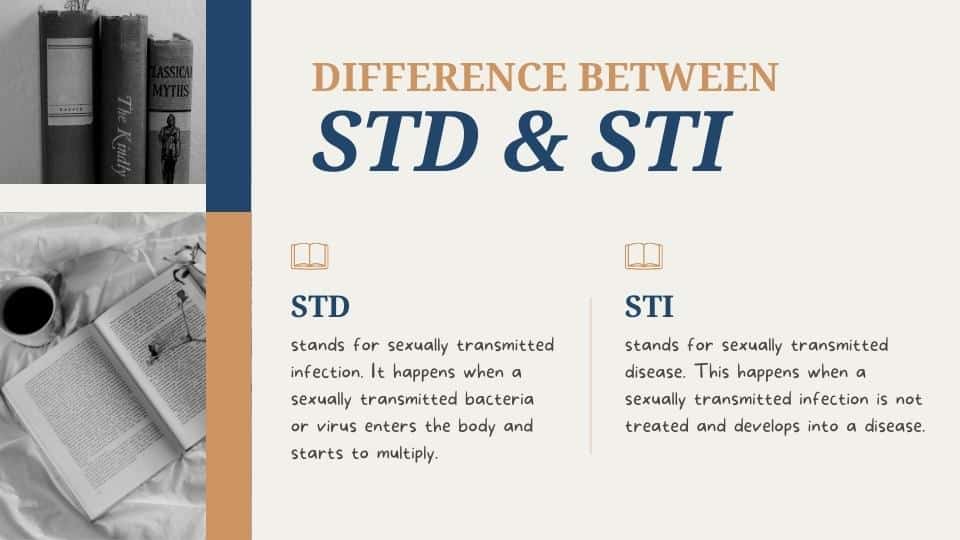
“STD” stands for sexually transmitted disease, while “STI” is short for sexually transmitted infection. You probably already knew that, and you are hoping to find out whether there is any functional or practical difference between the two terms. The answer is more complicated than it appears at first glance, primarily because not everyone in the medical field agrees. This article will discuss What’s the Difference Between STD and STI.
Diving Deeper: What Exactly Are Diseases and Infections?
Infection vs. disease
- Think of an infection as the first step on the road to disease. Infections haven’t yet turned into disease and often don’t cause any symptoms.
- This is actually why many experts are pushing to use STI over STD, and believe “STD” is misleading.
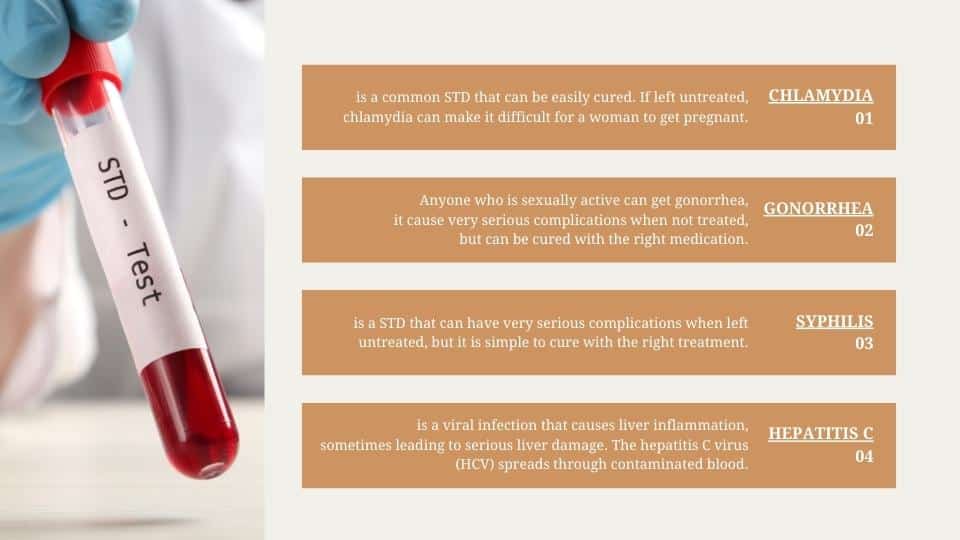
- “Disease” suggests that a person has a medical problem with obvious signs and symptoms. That’s often not the case at all since the most common STIs — like chlamydia and gonorrhea — are often asymptomatic.
- Another major difference between STDs and STIs is how they present. Because an STD is the later stage of an STI, you may have some symptoms. With an STI however, many carriers show no signs of being infected.
 All STDs start as STIs
All STDs start as STIs
- Not all diseases start as infections, but when it comes to sexually transmitted ones, they do.
- Infections occur when pathogens like viruses, bacteria, or parasites enter your body and start to multiply. How they get into your body depends on the type of pathogen.
- Some get in through skin-to-skin contact with a person who has an infection; others are transmitted through an exchange of bodily fluids, like semen, vaginal secretions, or blood.
- Infection progresses to disease when these pathogens cause damage to your cells, and signs and symptoms appear.
But not all STIs develop into STDs
- Some STIs never develop into STDs. Take HPV, for example.
- HPV usuallyTrusted Source clears up on its own without causing any health problems. In these cases, HPV is an STI.
- If the infection doesn’t clear on its own, it can cause genital warts or certain cancers. This then makes it a disease.
Common Symptoms of STIs and STDs
No two STIs or STDs are the same, but some have very similar symptoms. Common symptoms to watch out for include:
- Unusual discharge from the vagina or penis
- Pain while urinating
- Painful blisters around the genitals
- Fleshy growths around the genitals
- Tingling or itching around the genitals
- In men, pain in the testicles
- In women, pain in the pelvis or abdomen
- In women, irregular periods or bleeding after sex
- Two infections which have slightly more unusual symptoms are syphilis and HIV. The primary symptoms of syphilis can include one or more painless sores on the genitals, a rash and flu-like symptoms. The primary symptoms of HIV can include flu-like symptoms and a red rash across the body.
- Pubic lice and scabies, while not STIs or STDs in the strictest sense, are commonly spread through sexual contact and can cause genital itching, a rash, spots of blood on your genitals, and black spots in your underwear.
- It’s also very important to understand that not all STD and STI initially present with symptoms – in fact up to 70% of women don’t experience symptoms when infected with chlamydia. For that reason, you should get tested after any episodes of unprotected sex, even if you’re asymptomatic.
When to get tested
- have had sex without a barrier method, like a condom
- have had or are planning to have sex with a new partner
- have multiple sexual partners
- are worried you may have been exposed to an STI
- are pregnant
- share injection drug equipment
What happens next?
That depends on your results.
Negative Result
| If you receive a negative result, stay on top of screening with regular STI testing. |
| Ask your healthcare provider about the best screening schedule for you based on your individual risk factors. You can also talk to them about the best ways to reduce your risk for STIs, like using barrier methods or PrEP. |
Positive Result
| If you receive a positive result, your healthcare provider will prescribe a treatment or management plan depending on the diagnosis. |
| You’ll also need to notify your partner(s) so they can be tested and treated if needed. Not sure how to tell them? We’ve got you! This guide can help. |
| The most common STIs are caused by bacteria. A course of antibiotics can usually cure them. |
| Antibiotics don’t work on infections caused by viruses. Some viral infections clear on their own, but most are long-term conditions. Antiviral medications can usually manage symptoms and reduce the risk of transmission. |
| For STIs like crabs, which are caused by something other than bacteria or viruses, topical and oral medications usually do the trick. |
| Retesting might be recommended to make sure the treatment has worked. |
How can I protect myself from STIs?
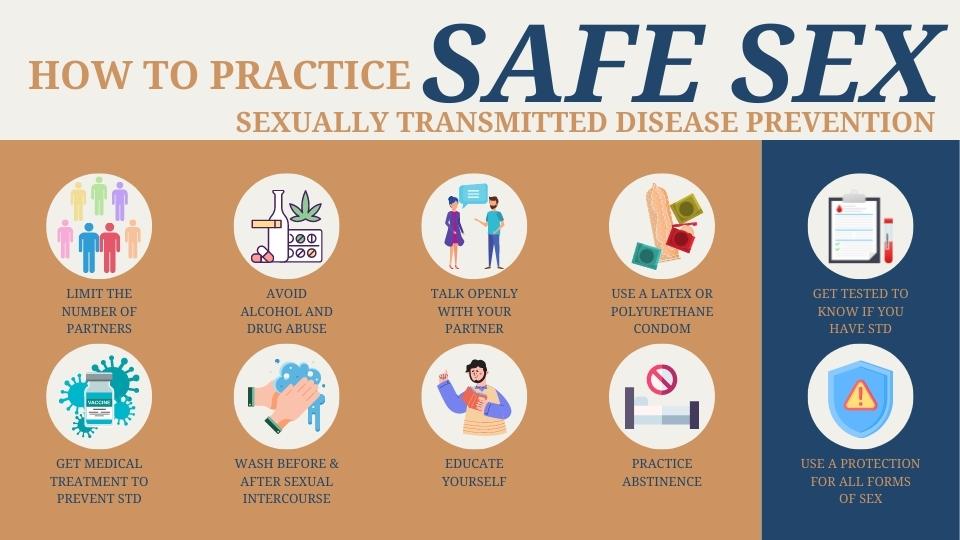
Only abstaining from sex (abstinence, or not having sex) offers complete protection from STIs. If you are sexually active, make sure to:
- Use a latex condom whenever you have any kind of sex. Condoms are especially important if you have multiple sex partners.
- Have sex with one person (monogamy). Or limit the number of sexual partners. Each new partner raises your risk of catching an STI.
- Choose sex partners carefully. Don’t have sex if you suspect your partner has an STI.
- Get checked for STIs regularly. Doing so helps prevent spreading the infection to other people. And ask any new sex partner to get tested before having sex for the first time.
- Avoid alcohol or drugs before having sex. People who are drunk or high may engage in risky sexual behaviors, which can lead to an STD.
- Learn the signs and symptoms of STIs. If you notice symptoms, get treatment quickly.
- Educate yourself about STIs. The more you know, the better you can protect yourself and your partners.
If I have an STD, how can I prevent spreading it to others?
Take steps to protect yourself and others:
- Don’t have sex until you see a healthcare provider and receive treatment. You can resume sex when your healthcare provider says it’s OK.
- Follow your healthcare provider’s instructions for treatment.
- Return to your healthcare provider to get rechecked.
- Be sure your sex partner or partners also receive treatment.
- Use condoms whenever you have sex, especially with new partners.
Conclusion
Not getting an STI test means remaining unaware of the presence of the infection. Therefore, that ultimately also increases the risk of transmitting it to other people. This may explain why more and more health organizations have trended toward embracing the term STI over STD in more recent years.
Most Commonly Sexually Transmitted Infections (STIs)

 All STDs start as STIs
All STDs start as STIs