PPE in HIV may occur even though people living with HIV often show no obvious symptoms during the early stages of infection. Over time, without consistent antiretroviral therapy (ART), the immune system gradually weakens, making the body more vulnerable to opportunistic infections and complications. One of the common conditions that frequently appears as a warning sign of immune deficiency is Pruritic Papular Eruption (PPE), also known as an “itchy papular rash in people with HIV.”
Although PPE itself is not directly life-threatening, it reflects the decline of immune health and can significantly impact quality of life. Persistent itching, physical discomfort, emotional stress, and worries about social appearance all contribute to the burden of this condition. Therefore, understanding PPE is crucial not only for patients but also for their families and communities.
PPE in HIV – Characteristics
PPE in HIV is a common skin condition that appears as itchy papules, often resembling mosquito or insect bites. The lesions are typically red and inflamed, and may develop pustules if secondary bacterial infection occurs after scratching. Dark spots or scars often remain once the lesions heal. More importantly, PPE in HIV is not just a simple rash but serves as a biological marker of declining immune function, signaling vulnerability to opportunistic infections and complications.

PPE in HIV – Pathogenesis
The exact cause of PPE in HIV is not fully understood, but research highlights several contributing mechanisms:
- Abnormal immune response: Weakened immunity causes the body to overreact to environmental stimuli such as insect bites or allergens.
- Chronic inflammation: HIV triggers ongoing cellular inflammation, making the skin more sensitive and irritable.
- Secondary infections: Scratching or minor skin breaks may lead to bacterial or fungal superinfections.
- Association with CD4 count: Patients with CD4 counts below 200 cells/µL are more likely to develop PPE.
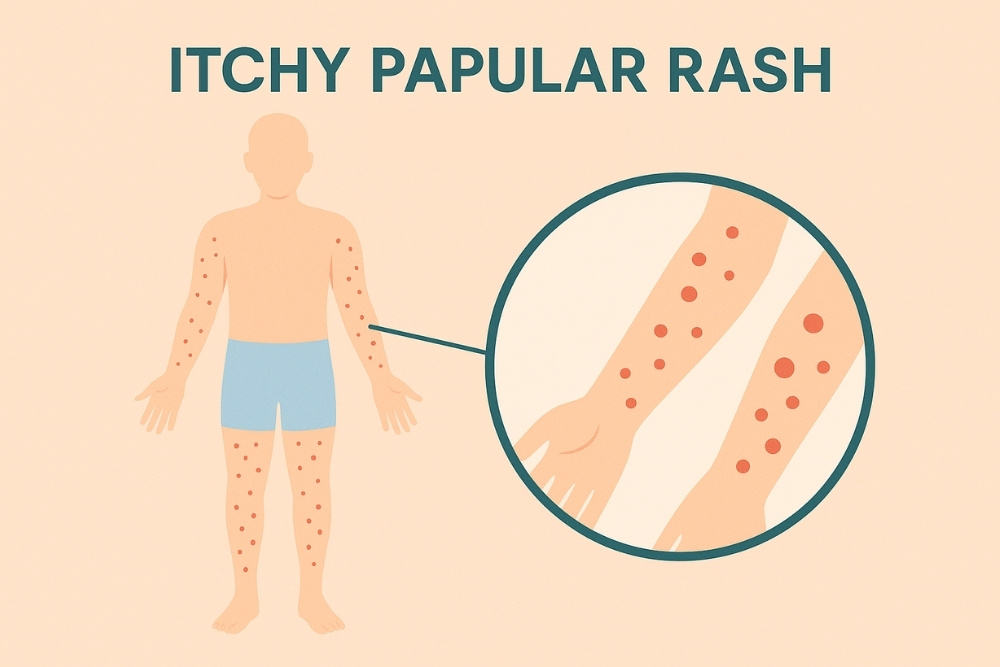
PPE in HIV – Clinical Features
Clinical presentations of PPE in HIV include:
- Itchy, red, or raised papules resembling insect bites
- Inflamed lesions with excoriations due to scratching
- Dark spots or scars left after lesions resolve
- Pustules when complicated by bacterial infection
- Common sites: arms, legs, trunk, and exposed skin; less commonly on the face
- Chronic nature with severe itching that disturbs sleep and affects daily life
PPE in HIV – Is It Contagious?
Many people wonder whether PPE in HIV is contagious. The answer is no—PPE itself is not a contagious condition. However, what must be taken seriously is HIV infection, which can be transmitted through blood, body fluids, and unprotected sexual contact. Direct skin-to-skin contact with PPE lesions will not spread the condition, but if someone comes into contact with blood, pus, or open wounds containing HIV and has cuts or sores of their own, there is a risk of HIV transmission.
What Happens If HIV Is Not Treated?
If a person living with HIV does not receive treatment, several serious outcomes can occur:
- Progressive destruction of the immune system, particularly CD4 cells
- Development of opportunistic infections such as tuberculosis, pneumonia, or oral thrush
- Higher risk of severe illnesses such as certain cancers, heart disease, and kidney disease
- Progression to AIDS, which can be life-threatening
Prevention
The most effective way to prevent PPE is to protect and maintain overall immune function:
- Get tested for HIV regularly to know your status early
- Begin antiretroviral therapy (ART) immediately after an HIV diagnosis
- Use condoms consistently during sexual activity
- Never share needles or syringes with others
- Care for your skin: avoid scratching, keep it moisturized, and prevent dryness or secondary infection
Treatment Approaches
Treatment for PPE focuses on relieving itching, preventing secondary infections, and controlling HIV:
- Antiretroviral therapy (ART): The cornerstone of treatment, restoring immune function and reducing the likelihood of PPE
- Antihistamines: Help relieve itching
- Topical corticosteroids: Reduce skin inflammation
- Skin care: Avoid scratching, use moisturizing creams, and maintain good hygiene
- Managing complications: If secondary bacterial infections occur, antibiotics may be prescribed under medical supervision
⚠️ It is important to note that PPE treatment mainly manages symptoms. Lasting improvement requires consistent HIV treatment with ART.
Related Article

PPE in HIV – Physical, Psychological and Social Impacts
Even though PPE is not fatal, it can negatively affect many aspects of life.
| Impact Area | Description | Examples |
|---|---|---|
| Physical | – Severe itching disrupts daily activities – Sleep disturbance from chronic itching – Risk of bacterial infection from scratching – Fatigue due to poor rest |
– Waking up at night from uncontrollable itching – Pustular lesions from scratching – Constant tiredness |
| Psychological | – Loss of self-confidence due to scars or dark spots – Stress and anxiety about health – Risk of depression if the condition is persistent |
– Avoiding wearing clothes that show skin – Withdrawing from social settings – Feeling hopeless or anxious |
| Social | – Misunderstanding as a contagious skin disease – Stigma or discrimination in society – Strained family and social relationships |
– Friends avoiding close contact – Exclusion from activities – Feeling isolated or rejected |
“The most important step in preventing PPE and other opportunistic conditions is consistent HIV treatment with antiretroviral therapy. ART helps control viral load, strengthen the immune system, and reduce the risk of complications.”
Conclusion
PPE in HIV is a common condition in people with weakened immune systems. It presents as chronic itchy papules that often leave scars or dark spots. While not directly life-threatening, PPE is a warning sign of immune decline. The best prevention is regular HIV testing, early initiation of ART, and strict adherence to medical advice. By doing so, people living with HIV can not only manage PPE but also maintain a healthier and more fulfilling life.
Reference:
↪︎ ตุ่ม HIV กับตุ่ม PPE ต่างกันอย่างไร วิธีสังเกตขึ้นที่ไหน?
↪︎ ตุ่ม PPE หรือตุ่มเอดส์ เมื่อเป็นแล้วควรดูแลตนเองอย่างไร?
↪︎ โรคเอดส์ (HIV/AIDS) ความรู้เรื่องอาการ ระยะ และการป้องกัน

