What is genital herpes?
Genital herpes is a sexually transmitted infection (STI). This STI causes herpetic sores, which are painful blisters (fluid-filled bumps) that can break open and ooze fluid in the genital area. Genital herpes passed on through vaginal, anal and oral sex. Treatment from a sexual health clinic can help. Symptoms clear up on their own but can come back.

Causes of genital herpes
Two types of the herpes simplex virus (HSV) cause genital herpes:

- HSV-1. This type usually causes cold sores, but it can also cause genital herpes.
- HSV-2. This type usually causes genital herpes, but it can also cause cold sores.
The viruses enter the body through skin abrasions or mucous membranes. Mucous membranes are the thin layers of tissue that line the openings of your body. They can be found in your nose, mouth, and genitals.
Once the viruses are inside, they incorporate themselves into your cells. Viruses tend to multiply or adapt to their environments very easily, which makes treating them difficult.
HSV-1 or HSV-2 can be found in bodily fluids, including:
- Saliva
- Semen
- Vaginal secretions
How common is genital herpes?
HSV II infection is more common in women and in people who have had more than five sexual partners. Most people with HSV II do not know they have it, because it does not always cause symptoms.
How is genital herpes spread?
You can get genital herpes by having vaginal, anal, or oral sex with someone who has the infection. You can get herpes if you have contact with:
- A herpes sore
- Saliva from a partner with an oral herpes infection
- Genital fluids from a partner with a genital herpes infection
- Skin in the oral area of a partner with oral herpes or
- Skin in the genital area of a partner with genital herpes
- You also can get genital herpes from a sex partner who does not have a visible sore or is unaware of their infection. It is also possible to get genital herpes if you receive oral sex from a partner with oral herpes
- You will not get herpes from toilet seats, bedding, or swimming pools. You also will not get it from touching objects, such as silverware, soap, or towels
How do I know if I have genital herpes?
Most people with genital herpes have no symptoms or have very mild symptoms. Herpes sores usually appear or more blisters on or around the genitals, rectum or mouth. By blisters break and leave painful sores that may take a week or more to heal. Flu-like symptoms (e.g., fever, body aches, or swollen glands) and can include an unusual sore, a smelly genital discharge, burning when peeing, or bleeding between periods (if you have a menstrual cycle).
Symptoms of genital herpes
The appearance of blisters is known as an outbreak. On average, a first outbreak will appear 4 daysTrusted Source after contracting the virus, However, it can take as little as 2 days, or as much as 12 days or more, to appear.
General symptoms for those with a penis include blisters on the:
- Penis
- Scrotum
- Buttocks (near or around the anus)
General symptoms for those with a vagina include blisters around or near the:
- Vagina
- Anus
- Buttocks
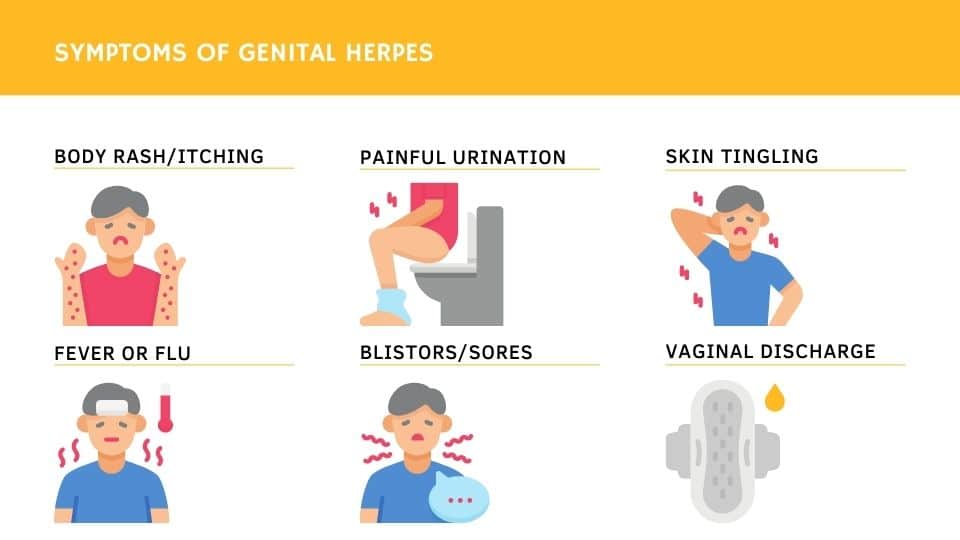
General symptoms for anyone include the following:
- Blisters may appear in the mouth and on the lips, face, and anywhere else that came into contact with areas of infection.
- The area that has contracted the condition often starts to itch, or tingle, before blisters actually appear.
- The blisters may become ulcerated (open sores) and ooze fluid.
- A crust may appear over the sores within a week of the outbreak.
- Your lymph glands may become swollen. Lymph glands fight infection and inflammation in the body.
- You may have headaches, body aches, and fever.
- General symptoms for a baby born with herpes (contracted through a vaginal delivery) may include ulcers on the face, body, and genitals.
Babies who are born with genital herpes can develop very severe complications and experience:
- blindness
- brain damage
- death
- It’s very important that you tell your doctor if you contract genital herpes and are pregnant.
- They will take precautions to prevent the virus from being transmitted to your baby during delivery. If you have herpes blisters along your birth canal, they may opt to deliver your baby via cesarean rather than a routine vaginal delivery.
When to see a doctor for genital herpes
However, if you do have symptoms of genital herpes, it’s important to see a doctor. They can make a diagnosis and discuss management strategies with you. Additionally, if you think you may have been exposed to genital herpes, or if you want a full STI exam and testing, you can schedule an appointment with your doctor. If you can’t make it to a doctor in person, you can also use an at-home test kit. However, an in-person test done by your doctor may be more accurate.
Diagnosing genital herpes
- Your doctor can typically diagnose a herpes transmission by a visual examination of the herpes sores. Although they aren’t always necessary, your doctor may confirm their diagnosis through laboratory tests.
- A blood test can diagnose herpes simplex virus before you experience an outbreak. However, it’s not always necessary to be screened for HSV-1 or HSV-2 if you haven’t been exposed to the virus and aren’t displaying any symptoms.
Treatment for genital herpes
There’s no cure. Symptoms clear up by themselves, but the blisters can come back (an outbreak or recurrence).
Treatment the first time you have genital herpes
- antiviral medicine to stop the symptoms getting worse – you need to start taking this within 5 days of the symptoms appearing
- cream for the pain
- If you have had symptoms for more than 5 days before you go to a sexual health clinic, you can still get tested to find out the cause.
Treatment if the blisters come back
- Antiviral medicine may help shorten an outbreak by 1 or 2 days if you start taking it as soon as symptoms appear.
- But outbreaks usually settle by themselves, so you may not need treatment.
- Recurrent outbreaks are usually milder than the first episode of genital herpes.
- Over time, outbreaks tend to happen less often and be less severe. Some people never have outbreaks.
- Some people who have more than 6 outbreaks in a year may benefit from taking antiviral medicine for 6 to 12 months.
- If you still have outbreaks of genital herpes during this time, you may be referred to a specialist.
Genital herpes and pregnancy
If you have genital herpes during pregnancy, there’s a risk your baby could develop a serious illness called neonatal herpes. This can be fatal, but most babies recover with antiviral treatment. The risk of your baby getting neonatal herpes is low if you have had genital herpes before. It’s higher if you get genital herpes for the first time in pregnancy.
Genital herpes treatment in pregnancy
You may be offered antiviral treatment:
- to treat outbreaks in pregnancy
- from 36 weeks to reduce the chance of an outbreak during birth
- from diagnosis until the birth if you first get herpes after 28 weeks of pregnancy
Many women with genital herpes have a vaginal delivery. You may be offered a caesarean, depending on your circumstances.
How to deal with outbreaks yourself
If you have been diagnosed with genital herpes and you’re having an outbreak:
Do
- keep the area clean using plain or salt water to prevent blisters becoming infected
- apply an ice pack wrapped in a flannel to soothe pain
- apply petroleum jelly (such as Vaseline) or painkilling cream (such as 5% lidocaine) to reduce pain when you pee
- wash your hands before and after applying cream or jelly
- pee while pouring water over your genitals to ease the pain
Don’t
- do not wear tight clothing that may irritate blisters or sores
- do not put ice directly on the skin
- do not touch your blisters or sores unless you’re applying cream
- do not have vaginal, anal or oral sex until the sores have gone away

Why genital herpes comes back
Genital herpes is caused by a virus called herpes simplex. Once you have the virus, it stays in your body. It will not spread in your body to cause blisters elsewhere. It stays in a nearby nerve and causes blisters in the same area.
- If you can, avoid things that trigger your symptoms.
- ultraviolet light – for example, from sunbathing or sunbeds
- friction in your genital area – for example, from sex (lubricant may help) or tight clothing
- smoking
- drinking alcohol
Protecting against genital herpes
The only way to completely avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting genital herpes:
- Being in a long-term mutually monogamous relationship with a partner who does not have herpes.
- Using condoms the right way every time you have sex.
- Be aware that not all herpes sores occur in areas that a condom can cover. Also, the skin can release the virus (shed) from areas that do not have a visible herpes sore. For these reasons, condoms may not fully protect you from getting herpes.
If your sex partner(s) has/have genital herpes, you can lower your risk of getting it if:
- Your partner takes an anti-herpes medicine every day. This is something your partner should discuss with his or her healthcare provider.
- You avoid having vaginal, anal, or oral sex when your partner has herpes symptoms (i.e., during an “outbreak”).
FAQ
What happens if I don’t receive treatment?
Genital herpes can cause painful genital sores and can be severe in people with suppressed immune systems.
If you touch your sores or fluids from the sores, you may transfer herpes to another body part like your eyes. Do not touch the sores or fluids to avoid spreading herpes to another part of your body. If you do touch the sores or fluids, quickly wash your hands thoroughly to help avoid spreading the infection.
If you are pregnant, there can be problems for you and your unborn fetus
Can I still have sex if I have herpes?
If you have herpes, you should talk to your sex partner(s) about their risk. Using condoms may help lower this risk but it will not get rid of the risk completely. Having sores or other symptoms of herpes can increase your risk of spreading the disease. Even if you do not have any symptoms, you can still infect your sex partners.
You may have concerns about how genital herpes will impact your health, sex life, and relationships. While herpes is not curable, it is important to know that it is manageable with medicine. Daily suppressive therapy (i.e., daily use of antiviral medication) can lower your risk of spreading the virus to others. Talk to a healthcare provider about your concerns and treatment options.
A genital herpes diagnosis may affect how you will feel about current or future sexual relationships. Knowing how to talk to sexual partners about STDsexternal icon is important.
Problems With Herpes
People often don’t have serious problems from herpes, but there’s a chance of them. Wash your hands often, especially during an outbreak. If you touch a blister and rub your eyes, the infection can spread to your eyes. If your eyes are red, swollen, hurt, or are sensitive to light, see your doctor. Treating it can help prevent serious vision problems.
Shingles, also called herpes zoster, is caused by the varicella zoster virus (VZV), which causes chickenpox earlier in life. The natural history of varicella zoster infection is similar to genital herpes infection in that VZV also becomes latent in the sensory nerve roots. Later in life the virus may exit, causing shingles.
Recurrences in shingles cause blister lesions in a single area of skin called a dermatome. Shingles is not a sexually transmitted infection and is independent from genital herpes.
What is the link between genital herpes and HIV?
Herpes infection can cause sores or breaks in the skin or lining of the mouth, vagina, and rectum. This provides a way for HIV to enter the body. Even without visible sores, herpes increases the number of immune cells in the lining of the genitals. HIV targets immune cells for entry into the body. Having both HIV and genital herpes increases the chance of spreading HIV to a HIV-negative partner during oral, vagina, or anal sex.
References
- Genital Herpes – CDC Fact Sheet https://www.cdc.gov/std/herpes/stdfact-herpes.htm
- Genital herpes https://www.nhs.uk/conditions/genital-herpes/
- Genital Herpes https://www.healthline.com/health/std/genital-herpes
- Genital Herpes Symptoms, Pictures, and Treatment https://www.webmd.com/genital-herpes/ss/slideshow-genital-herpes
- Genital Herpes https://www.hopkinsmedicine.org/health/conditions-and-diseases/herpes-hsv1-and-hsv2/genital-herpes
Last Updated on 24/10/2024 by ทีมที่ปรึกษา มูลนิธิเพื่อรัก