What is Bacterial Vaginosis (BV)?
Bacterial vaginosis (BV) is an infection of the vagina. It results from a change in the normal balance of vaginal bacteria.
BV usually doesn’t cause any other health problems. But it can lead to issues, especially when you’re pregnant or trying to get pregnant.
BV is a disturbance in the mix of bacteria in the vagina. Normally there is a healthy mix of millions of ‘friendly’ germs (bacteria) in our bodies, including in the vagina – we rely on them being there and they are a part of what keeps us healthy. In BV, the balance of vaginal bacteria is altered.
The type of bacteria called anaerobic bacteria (bacteria that grow in an environment without air) increase in number, whilst another type, called lactobacilli, dies off. This disturbance in the bacteria makes the inside of the vagina slightly less acidic than usual. This slight reduction in acidity then encourages the growth of more anaerobic bacteria and fewer lactobacilli.
Although the changes of BV don’t usually cause pain or itching, they do tend to cause a discharge which can smell stronger than usual. Sometimes it smells ‘fishy’, particularly after sexual intercourse. It can be watery and grayish in color. This can be distressing and make women feel unclean. Some women then try to douche or wash themselves with soaps or perfumes – but this will only disturb the vagina more (because soaps are too alkaline for the inside of the vagina) and will make the problem worse.

What causes Bacterial Vaginosis?
Bacterial vaginosis — usually called BV — is a bacterial infection. It happens when the different kinds of healthy bacteria in your vagina get out of balance and grow too much. BV is often caused by gardnerella vaginalis, the most common type of bacteria in your vagina.
Anything that changes the chemistry of your vagina’s pH balance can mess with bacteria levels and lead to infection — like douching or using vaginal deodorants and other irritating products. Learn more about keeping your vagina healthy.
Bacterial vaginosis isn’t a sexually transmitted infection. But having sex with a new partner, or multiple partners, may increase your risk for BV. And sex sometimes leads to BV if your partner’s natural genital chemistry changes the balance in your vagina and causes bacteria to grow.
How is Bacterial vaginosis spread?
Although it is not clear how BV is transmitted, it is more common in women who are sexually active. It sometimes develops soon after intercourse with a new partner. Women who have female sexual partners may be at higher risk than women who have sex with only male partners.
Research has not conclusively found a link between BV and specific sexual practices or acts. However, recent evidence supports the use of condoms to reduce the risk of this infection.
BV rarely affects those who have never had sex.
You cannot get BV from toilet seats, bedding, or swimming pools.
Risk factors for bacterial vaginosis include:
- Having multiple sex partners or a new sex partner. Doctors don’t fully understand the link between sexual activity and bacterial vaginosis, but the condition occurs more often in women who have multiple sex partners or a new sex partner. Bacterial vaginosis also occurs more frequently in women who have sex with women.
- Douching. The practice of rinsing out your vagina with water or a cleansing agent (douching) upsets the natural balance of your vagina. This can lead to an overgrowth of anaerobic bacteria, and cause bacterial vaginosis. Since the vagina is self-cleaning, douching isn’t necessary.
- using certain feminine hygiene products, such as vaginal deodorants and douches
- using a perfumed bubble bath
- using some scented soaps
- bathing in water that contains antiseptic liquids
- washing underwear with a strong detergent
- smoking
- Natural lack of lactobacilli bacteria. If your natural vaginal environment doesn’t produce enough of the good lactobacilli bacteria, you’re more likely to develop bacterial vaginosis.
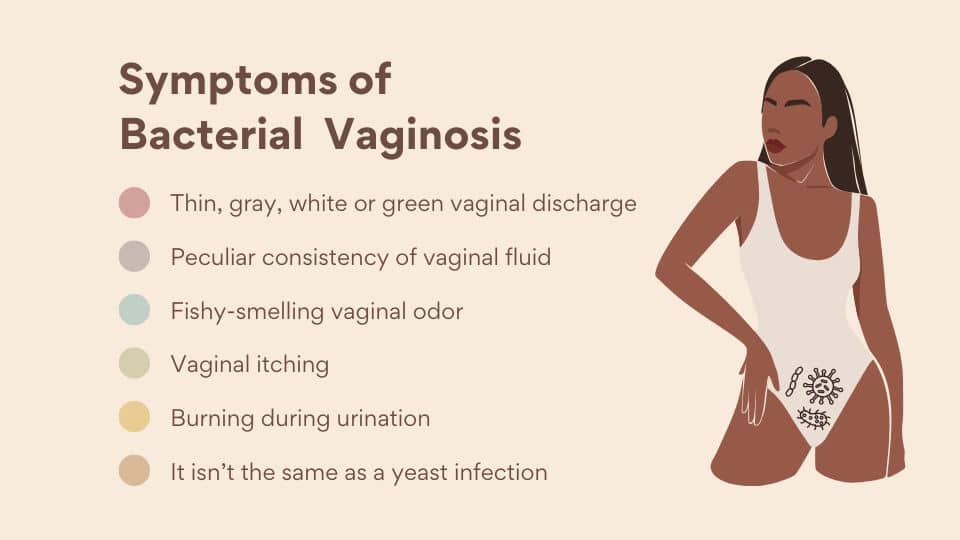
Bacterial Vaginosis Symptoms
About half of the time, women with BV have no symptoms. But they can include:
- Burning feeling when you pee
- Fishy smell that gets stronger after sex
- Itching
- Thin white, gray, or green discharge
- It isn’t the same as a yeast infection. Those often have a thick white discharge that doesn’t smell.
Complications
Bacterial vaginosis doesn’t generally cause complications or itself is not harmful, but it can increase the riskTrusted Source of other health issues.
General health complications
- Sexually transmitted infections (STIs). Having bacterial vaginosis makes women more susceptible to sexually transmitted infections, such as
- Herpes
- Human Papilloma Virus, better known as HPV
- Chlamydia
- gonorrhea
- HIV, as having BV increases a person’s susceptibility to the virus
- a post surgical infection, for example after some types of abortion or a hysterectomy
Pregnancy complications
- early or preterm delivery. In pregnant women, bacterial vaginosis is linked to premature deliveries and low birth weight babies.
- loss of pregnancy
- the amniotic sac breaking open too early
- postpartum endometritis, which is irritation or inflammation of the lining of the uterus after delivery
- chorioamnionitis, which is inflammation of the membranes around the fetus
Chorioamnionitis significantly increases the chance of an early delivery. If the newborn lives, they have a higher risk of cerebral palsy.
Fertility complications
BV may directly increase the likelihood of difficulty conceiving. And it may increase the risk of health complications that can affect fertility.
- Tubal factor infertility: This is infertility caused by damage to the fallopian tubes, which connect the ovaries to the uterus.
- Pelvic inflammatory disease (PID). Bacterial vaginosis can sometimes cause PID, an infection of the uterus and the fallopian tubes that can have serious effects, including infertility.
- Unsuccessful in vitro fertilization (IVF): If a person has BV, any IVF treatments may be less likely to succeed.
- Infection risk after gynecologic surgery. Having bacterial vaginosis may increase the risk of developing a post-surgical infection after procedures such as hysterectomy or dilation and curettage (D&C).
When to see a doctor
- You have vaginal discharge that’s new and associated with an odor or fever. Your doctor can help determine the cause and identify signs and symptoms.
- You’ve had vaginal infections before, but the color and consistency of your discharge seems different this time.
- You have multiple sex partners or a recent new partner. Sometimes, the signs and symptoms of a sexually transmitted infection are similar to those of bacterial vaginosis.
- You try self-treatment for a yeast infection with an over-the-counter treatment and your symptoms persist.
Diagnosis of Bacterial Vaginosis
Bacterial Vaginosis Diagnosis The doctor will:
- Ask about your medical history
- Do an overall physical exam
- A doctor’s evaluation
- Examination of a sample of the discharge and/or fluid from the cervix
- If girls or women have a vaginal discharge that is unusual or that lasts for more than a few days, they should see a doctor.
- Doctors suspect bacterial vaginosis based on symptoms, such as a gray discharge that smells fishy. They then ask questions about the discharge and possible causes (such as sexually transmitted diseases).
- To confirm the diagnosis, doctors do a pelvic examination. While examining the vagina, the doctor takes a sample of the discharge with a cotton-tipped swab. The sample is examined under a microscope. With information from this examination, the doctor can usually identify the microorganism causing the symptoms. If test results are inconclusive, other newer tests can be done using the samples obtained during the pelvic examination.
- Usually, the doctor also uses a swab to take a sample of fluid from the cervix (the lower part of the uterus that opens into the vagina). This sample is tested for sexually transmitted diseases.
- To determine whether there are other infections in the pelvis, the doctor checks the uterus and ovaries by inserting the index and middle fingers of one gloved hand into the vagina and pressing on the outside of the lower abdomen with the other hand. If this maneuver causes substantial pain or if a fever is present, other infections may be present.
How is Bacterial vaginosis treated?
BV sometimes clears up without treatment. However, the symptoms can resemble those of other health issues, such as gonorrhea or trichomoniasis. And untreated BV can lead to complicationsTrusted Source, especially during pregnancy.
For these reasons, getting a professional diagnosis is key to ensure that the treatment is successful.
BV may also increase the risk of complications following a hysterectomy or some types of abortion. Some doctors recommend giving BV treatment to everyone who has these procedures, regardless of whether they have BV symptoms.
Male partners do not usually require treatment. However, BV can transmit from a male to multiple female sexual partners.
Below, we explore some treatment options for BV.
Antibiotic medication
Antibiotics are effective in up to 90%Trusted Source of BV cases, but the condition often comes back again within a few weeks.
Below are some antibiotic medications that a doctor may prescribe for BV.
Metronidazole
Metronidazole is the most common antibiotic treatment for BV.
It is available in these forms:
- Oral tablets: People typically take these twice daily for 7 days. Doctors consider tablets the most effective treatment, especially if the person is breastfeeding or pregnant.
- Single dose: The Food and Drug Administration (FDA) approved Solosec (secnidazole) in 2017 for the treatment of BV. This is the only single-dose oral BV treatment. A person sprinkles a 2-gram (g) packet onto food.
- Gel: A person applies this gel into their vagina once a day for 5 days.
Metronidazole interacts harmfully with alcohol. This combination can make a person seriously unwell and cause side effects such as nausea and vomiting.
Clindamycin
Clindamycin is an alternative antibiotic. It may work if metronidazole is not effective or if the infection recurs.
Clindamycin cream is the first-line treatment that a person applies inside their vagina. A person does this at bedtime for 7 daysTrusted Source.
Instead, doctors may prescribe clindamycin tablets, which a person takes twice a day for 7 days, or clindamycin ovules, which a person inserts into their vagina at bedtime for 3 days.
Clindamycin ovules and cream weaken latex, so barrier methods of contraception may be less effective during the treatment.
Some examples of these methods include:
- latex condoms
- diaphragms
- cervical caps
The FDA has recently approved a new clindamycin gel, Xaciato, for the treatment of BV in females aged 12 years and older.
Learn more about the dosage and application of metronidazole and clindamycin here.
Tinidazole
Tinidazole is another antibiotic that can treat BV if metronidazole does not work or if the condition recurs. A person takes a 2-g oral doseTrusted Source once a day for 2 days. Or, they take a 1-g dose once a day for 5 days. Anyone using this medication should avoid alcohol and take their doses with food to minimize the risk of gastrointestinal side effects.
Alternatives to antibiotics for bacterial vaginosis
Yogurt
Some women with BV say that things settle more quickly and symptoms are eased by applying a thin coat of plain, live yogurt to the outside of the vagina daily, and by applying a small amount of plain live yogurt on a tampon for internal use before bed.
The evidence that live yogurt is helpful in treating or preventing BV is mixed, with some trials saying that it is helpful and some saying that it is not helpful. Overall specialists feel that there is not enough evidence in its favor to suggest it over other treatments.
Astodrimer sodium gel
Astodrimer sodium gel is a new kind of treatment for BV. It can be bought without a prescription online as Betafem® BV gel. It treats BV by creating a physical barrier that repels bacteria from coming close to and sticking to the vaginal wall. A 2019 trial showed that astodrimer gel once daily for seven days was well tolerated by women and provided rapid improvement in BV symptoms. Patients improved, or were cured at the same rate as with conventional antibiotics.
Vaginal acetic and lactic acid
Treatment with acetic and lactic acid gels aims to keep the vaginal pH at less than 4.5, to encourage lactobacilli to grow, and to discourage anaerobic bacteria from growing. Some studies have suggested that long-term use of vaginal acidifiers of this type reduces recurrences of BV. However, other studies suggest that this treatment, whilst harmless, is not effective.
Lactobacillus tablets
Lactobacillus suppositories and oral tablets are sold in some health food shops, for use in BV.
Orally consumed probiotics are believed to reach the vagina via the bowel. There is some evidence that this can be helpful in treatment and in prevention of BV. These studies suggest treatment needs to continue for at least two months. Other studies don’t show a clear benefit. Overall, specialists feel that there is not enough evidence in its favor to suggest it over other treatments.
Intravaginal lactobacillus treatment seems as though it ought to be an obvious solution – why not put the right bacteria where they are meant to go? However, results of studies on vaginal treatments with lactobacilli are also mixed, with some studies suggesting this treatment is effective and others not.
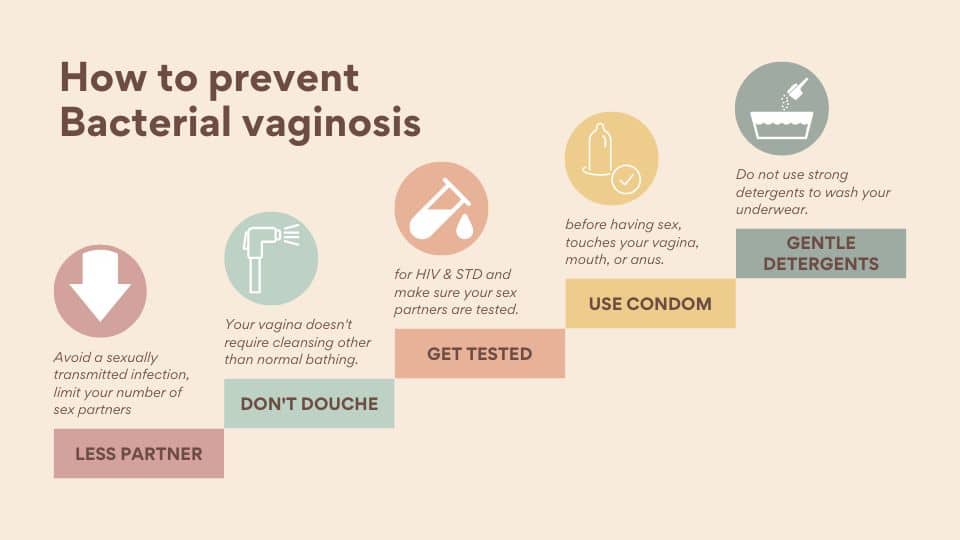
How to prevent Bacterial vaginosis
- Minimize vaginal irritation. Use mild, non deodorant soaps and unscented tampons or pads.
- Don’t douche. Your vagina doesn’t require cleansing other than normal bathing. Frequent douching disrupts the vaginal balance and may increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Avoid a sexually transmitted infection. Use a male latex condom, limit your number of sex partners or abstain from intercourse to minimize your risk of a sexually transmitted infection.
- Clean sex toys after every use.
- Do not push water into your vagina to clean it (douching). The vagina needs no specific cleaning.
- Get tested for sexually transmitted diseases, and make sure your sex partners are tested.
- Limit your number of sex partners.
- If your partner is male, put a condom on their penis before it touches your vagina, mouth, or anus.
- Use only water or mild soap to wash your genitals.
- Wipe from front to back after you use the bathroom.
- washing underwear in gentle detergents Do not use strong detergents to wash your underwear.
- Do not add bath oils, antiseptics, scented soaps, perfumed bubble bath, shampoos, etc, to bath water.
- Lighter periods seem to make BV less likely to return, so if you have heavy periods and are considering seeking treatment, this might be another reason to do so.
References
Bacterial Vaginosis https://my.clevelandclinic.org/health/diseases/3963-bacterial-vaginosis
Bacterial vaginosis https://www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/symptoms-causes/syc-20352279
Bacterial Vaginosis https://www.webmd.com/women/guide/what-is-bacterial-vaginosis
What is bacterial vaginosis? Symptoms and causes https://www.medicalnewstoday.com/articles/184622
Bacterial Vaginosis (BV) https://www.msdmanuals.com/home/women-s-health-issues/vaginal-infections-and-pelvic-inflammatory-disease/bacterial-vaginosis-bv
Bacterial Vaginosis
https://patient.info/sexual-health/vaginal-discharge-female-discharge/bacterial-vaginosis