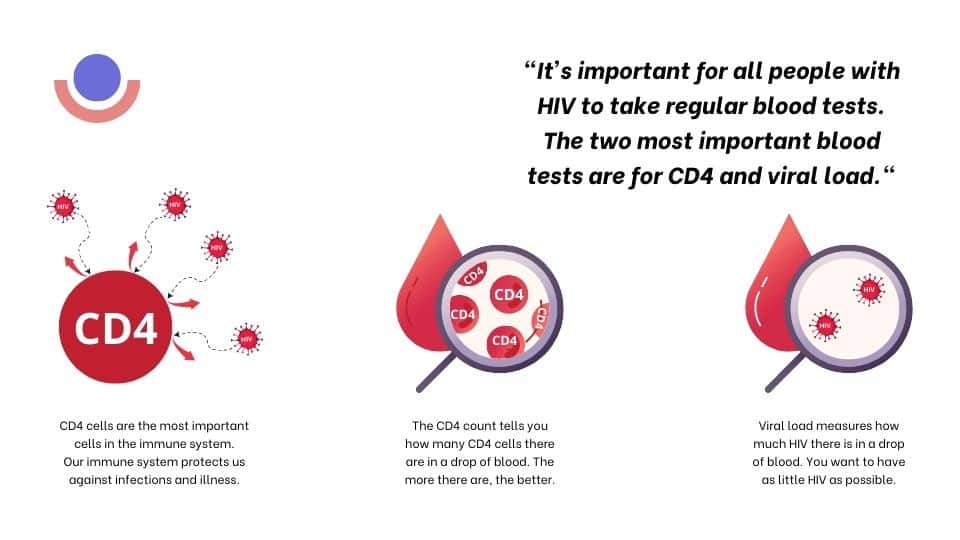
If an HIV infection has been confirmed, tests are routinely performed to determine the status of a person’s immune system and the level of viral activity in the body.
These are expressed in what is known as your CD4 and Viral Load.
List of contents
- What is a CD4 count?
- When a person is living with HIV
- What causes a CD4 count to drop?
- What are other factors that affect CD4 count?
- What is a viral load?
- How CD4 and viral load are related
- Getting tested
- How often should you test your CD4 counts?
- How often should you test your viral load counts?
- Why is it important to get tested regularly?
- Goals of Viral Suppression
- Benefits of Viral Control
These values give them and their healthcare team important information about:
- the health of their immune system
- the progression of HIV in their body
- how their body responds to HIV therapy
- how the virus itself responds to HIV therapy
The aim of treatment is to raise the CD4 count and lower the viral load. When viral levels become undetectable, the virus is no longer transmittableTrusted Source during sexual activity, according to the Centers for Disease Control and Prevention (CDC).
Regular testing can also ensure levels stay undetectable, and this can boost the person’s quality of life.
What is a CD4 count?
A CD4 count is a blood test to check the amount of CD4 cells in the body. CD4 cells are a type of white blood cell. They play a key role in the immune system. They alert other immune cells to the presence of infections such as bacteria and other viruses in the body. CD4 cells are also a subset of immune cells called T cells.
The CD4 test is one of the more familiar testing assays known to people with HIV. The test measures the level of CD4 helper T-cells in the blood—cells that are not only vital to immune function but are the primary target of HIV infection. As HIV gradually depletes these cells, the body becomes less able to defend itself against a widening range of opportunistic infections.
When a person is living with HIV
the virus attacks the CD4 cells in their blood. This process damages CD4 cells and causes a drop in the number of them in the body, making it difficult to fight infections. Monitoring CD4 cells is important for people who are receiving treatment for HIV.
CD4 counts vary widely. For many people, however, the higher a CD4 count is when they receive a diagnosis and start treatment, the more quickly they are likely to see it rise as a result of therapy. This is one reason why an early diagnosis is essential.
The chart below summarizes the ranges of CD4 counts:
CD4 count Meaning
500–1,600 cells/mm3 Most people without HIV have this level.
250–500 cells/mm3 The immune system is compromised, and one reason could be HIV.
Under 200 cells/mm3 A doctor will diagnose AIDS.
CD4 counts show the robustness of the immune system. A healthy immune system normally has a CD4 count ranging from 500 to 1,600 cells per cubic millimeter of blood (cells/mm3), according to HIV.gov.
When a CD4 count is lower than 200 cells/mm3, a person will receive a diagnosis of AIDS. AIDS is a separate condition that can develop in a person with HIV. It is also called stage 3 of HIV. At this stage, the body’s immune system is weak due to the low number of CD4 cells available to fight disease, and the person’s risk of infection is very high.
Today, the CD4 count is used to predict disease outcome as much as to measure an individual’s relative immune strength. By way of example, the CD4 nadir (the lowest point to which the CD4 count has dropped) is predictive of long-term morbidity, with lower values suggesting an increased risk of HIV-related and non-HIV-related illnesses, as well as slower immune recovery.
What causes a CD4 count to drop?
CD4 cells are part of the immune system. They are present in blood cells and help protect the body from disease. When HIV enters body cells, it reproduces or makes copies of itself. As it does so, it causes CD4 cells to die, leaving the body more prone to infection and disease.
Typically, the more virus that’s in the body, the lower the levels of CD4 will be, the more the immune system will be compromised, and the higher the person’s risk of infection.
Antiretroviral treatment suppresses the virus and gives CD4 cells a chance to recover. As a person receives treatment, they can expect CD4 levels to rise. In the first year of antiretroviral treatment, you can expect typically to see a person’s CD4 count rise by 50–150 cells/mm3. After that, there will be slower yearly increases.
What are other factors that affect CD4 count?
HIV is not the only factor affecting CD4 levels.
The following can also have an impact:
- Circadian rhythms, also called the body clock, vary during the day. One result of this is that CD4 levels tend to be lower in the morning and higher as the day progresses.
- Having an infection, such as the flu, pneumonia, or hepatitis B, can cause CD4 levels to fall.
- Some treatments, such as chemotherapy or single-dose steroids can cause CD4 levels to drop. However, ongoing steroid use may increase CD4 levels.
Other factors that may play a role include:
- stress
- fatigue
- nicotine or alcohol use
- Pregnancy
For this reason, there may be some variation in CD4 levels, even if a person’s health status has not changed. Also, the CD4 level will not affect how a person feels. Some people have low CD4 levels and function well, while others experience complications despite having higher levels.
What is a viral load?
While the CD4 count is an indicator of immune status and treatment efficacy, the viral load is arguably the more important measure when antiretroviral therapy begins.
The viral load measures the concentration of virus in the blood, also known as your “viral burden.” Labs will use a genetic testing technology—typically, the polymerase chain reaction (PCR) or a bDNA (branched DNA)—to quantify the number of viral particles in a milliliter (mL) of blood. HIV viral loads can range from undetectable (below the detection levels of current testing assays) to the tens of millions.
An HIV viral load test measures the number of HIV particles in a milliliter (mL) of blood. These particles are also known as “copies.” The test assesses the progression of HIV in the body. It’s also useful in seeing how well a person’s HIV therapy is managing the virus in their body.
What happens if you have a high viral load?
A person may have a high viral load soon after contracting HIV or if treatment is not proving effective. When a person first contracts the virus, levels will rise significantly, but in the next 3 to 8 weeks, the body starts to produce antibodies. This can reduce the virus levels. A viral load can include over a millionTrusted Source copies per mL of blood, especially after recent exposure
- Effective treatment will result in viral suppression. This is when there are fewer than 200Trusted Source copies/mL. At this stage, the risk of HIV progressing is low, but the virus is still present A person can still pass on the virus.
- As treatment progresses, the viral load can become so low that it is undetectable in a test. An undetectable viral load will be under 40 to 75 copies in a blood sample. This means there are relatively few copies of HIV in the blood.
- When this happens, it is no longer possible to pass the virus on to another person during sex, according to the CDCTrusted Source. An undetectable amount of HIV is untransmittable.
An undetectable result does not mean there is no virus in your blood or you have been “cleared” of infection. Undetectable simply means that the virus population has fallen below testing detection levels in blood but may be detectable elsewhere, such as in the semen.
However, continued treatment is necessary to ensure the viral load remains undetectable.
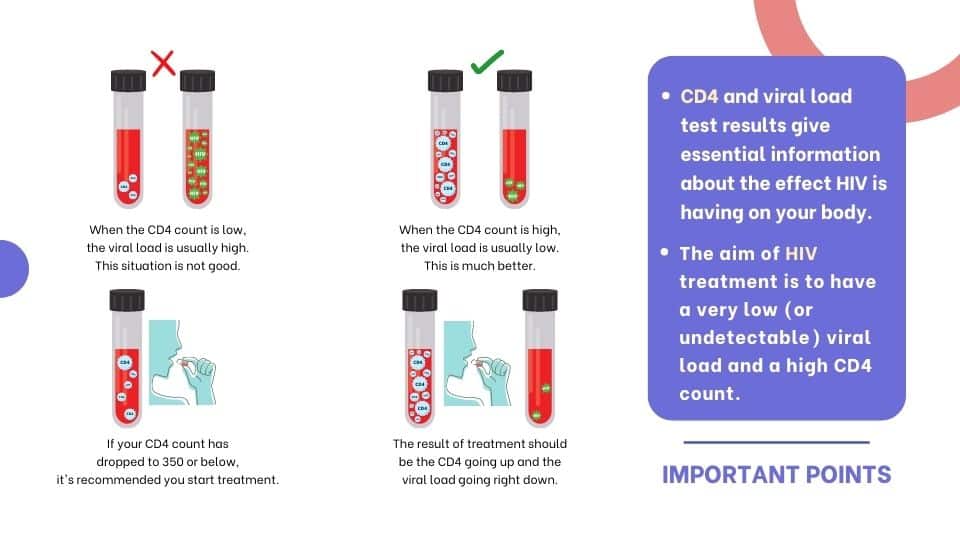
How CD4 and viral load are related
The CD4 and viral load tests measure different things. But the pattern of results for both tests are usually related.
When viral load is low or going down, CD4 counts will be higher or going up.
When CD4 counts are low or going down, viral load will be high or going up.
A few weeks after infection, HIV viral load is very high, and the CD4 count drops. Then as the immune system brings viral load down, CD4 counts go back up again.
There is sometimes a time lag between CD4 and Viral Load changes:
After starting HIV treatment (ART) viral load drops quickly. The CD4 count only increases slowly (often over several months).
If treatment fails and the viral load level starts to rebound, the CD4 count may take a while before it starts to fall.
As viral load gets higher, the CD4 count will nearly always start to fall within a few weeks.
Getting tested
Most people living with HIV will have regular CD4 and viral load tests, but the frequency will vary, according to how their treatment progresses and how their body responds to it.
How often should you test your CD4 counts?
Most people will need a test every 3 to 6 months, according to the U.S. Department of Health and Human Services.
More frequent testing may be needed if:
- you are just starting treatment
- you change medications
- your have a viral load that is difficult to suppress
CD4 status Need for testing
Most people with detectable virus. Every 3–6 months
HIV responds well to treatment, and CD4 levels have been stable between 300–500 cells/mm3 for 2 years. Every 12 months
Viral load remains undetectable, and CD4 counts are over 500 cells/mm3 for 2 years. May be optional
However, if any change occurs in the person’s health or treatment status, the doctor will review the testing schedule.
How often should you test your viral load counts?
The frequency of testing will depend on how soon after the diagnosis it is, the treatment, and how well the body is responding.
Status Frequency of testing
The person has just started antiretroviral treatment or their doctor has changed their treatment. After 2–8 weeks
Until the viral load becomes undetectable. Every 4–8 weeks
While the viral load is stable. Every 3–4 months
After levels remain stable for 2 years. Up to 6 months interval
Why is it important to get tested regularly?
CD4 and viral load testing can help you and your doctor understand:
- how well treatment is working
- your risk of developing an opportunistic infection
- the risk of HIV progressing to AIDS
- The results can guide decisions about future testing and treatment strategies.
Goals of Viral Suppression
The aim of antiretroviral therapy is to achieve viral suppression, defined as having fewer than 200 copies of HIV per millilter of blood.
- Greater treatment durability
- A lower risk for the development of drug-resistant virus
- Better clinical outcomes correlating to increased life expectancy
- The reduction of HIV transmission to no risk to an uninfected sexual partner (a strategy popularly referred to as treatment as prevention (TasP)
On the other hand, an increase in the viral load can often be an indication of treatment failure, poor drug adherence, or both.
It’s important to note that drug adherence of at least 80% to 85% is required to ensure viral suppression to undetectable levels. Uneven adherence not only reduces a person’s ability to achieve this, it increases the likelihood of treatment failure by allowing a drug-resistant virus to develop. This cause-effect relationship is the reason adherence should always be checked before therapy is changed.
That said, incidental variations in viral load (or “blips”) can occur even among those with 100% adherence. These are usually minimal and should not be the cause for alarm.
Regular monitoring of the CD4 count and viral load is recommended. Patients able to sustain CD4 counts over 500 cells/µL may be tested occasionally as directed by treating doctor.

Benefits of Viral Control
People with undetectable viral loads who achieved a CD4 count of 350 cells/µL or more within a year of starting therapy were likely to have a normal life expectancy. On the flip side, failure to achieve viral suppression reduced life expectancy by as much as 11 years.
References
CD4 vs. Viral Load: What’s in a Number?
- healthline.com/health/hiv-aids/cd4-viral-count
What to Know About Your CD4 Count and Viral Load
- verywellhealth.com/what-does-a-cd4-count-and-viral-load-mean-48630
How CD4 and viral load are related
- i-base.info/ttfa/section-2/14-how-cd4-and-viral-load-are-related/