Genital warts are small growths that develop around the genitals or anus. They are also known as venereal warts, or condylomata acuminata.
Genital warts affect the moist tissues of the genital area. They can look like small, flesh-colored bumps or have a cauliflower-like appearance. In many cases, the warts are too small to be visible. The warts form separately or in clusters. They may be small, at 5 millimetersTrusted Source or less, though in some cases they develop into large masses. The warts are usually skin-colored or somewhat darker.
List of contents
- What are genital warts?
- What causes Genital Warts?
- Risk factors for genital warts
- What are the symptoms of genital warts?
- Complications
- When to see a doctor
- How are genital warts diagnosed?
- How is Genital Warts treated?
- How to prevent Genital Warts
- How Long Do Genital Warts Last?
- When Is Someone With Genital Warts No Longer Contagious?
What are genital warts?
Genital warts develop on the skin and mucous membranes in the genital or anal area.
- In males, this includes the penis, scrotum, and anus.
- In females, this includes the vulva, the internal surface of the vagina, the cervix, and the anus.
Genital warts are not usually painful, but they can cause itching, redness, or discomfort, and they may bleed. Learn about the duration of outbreaks here.
If the warts do appear, it may be 3 weeks, several months, or even years after the person has developed the infection.
Genital warts are benign, or noncancerous.
What causes Genital Warts?
Genital warts are usually a sexually transmitted disease (STD). They’re caused by HPV (human papillomavirus). This virus also can cause some types of cancer. But the types of HPV that cause genital warts do not usually cause cancer.
Genital warts, like other warts, are caused by certain types of HPV. There are more than 100 different types of the virus, but only types 6 and 11 Trusted Source cause genital warts.
Genital warts are almost always spread through sexual contact. Your warts don’t have to be visible for you to spread the infection to your sexual partner.
However, the virus doesn’t always lead to complications such as genital warts. In fact, in most cases, the virus goes away on its own without causing any health problems.
Genital warts are usually caused by strains of HPV that differ from the strains that cause warts on your hands or other parts of the body.

Risk factors for genital warts
Most people who are sexually active get infected with genital HPV at some time. Factors that can increase your risk of becoming infected include:
- Having unprotected sex with multiple partners
- Having had another sexually transmitted infection
- Having sex with a partner whose sexual history you don’t know
- Have weakened immune systems
- Having a compromised immune system, such as from HIV or drugs from an organ transplant
- Becoming sexually active at a young age /are under the age of 30
- having other viral infections, such as HIV or herpes
- experiencing stress
- smoke
What are the symptoms of genital warts?
Genital warts are transmitted through sexual activity, including oral, vaginal, and anal sex. You may not start to develop warts for several weeks or months after infection.
Genital warts aren’t always visible to the human eye. They may be very small and the color of the skin or slightly darker. The top of the growths may resemble a cauliflower and may feel smooth or slightly bumpy to the touch.
They may occur as a cluster of warts, or just one wart.
For people assigned male at birth, genital warts may appear in the following areas:
- penis
- scrotum
- groin
- thighs
- inside or around the anus
For people assigned female at birth, these warts may appear:
- inside of the vagina or anus
- outside of the vagina or anus
- on the cervix
- Genital warts may also appear on the lips, mouth, tongue, or throat of a person who has had oral sexual contact with a person who has HPV.
Even if you can’t see genital warts, they may still cause symptoms, such as:
- vaginal discharge
- burning
- If genital warts spread or become enlarged, the condition can be uncomfortable or even painful.
- Small, flesh-colored, brown or pink swellings in your genital area
- A cauliflower-like shape caused by several warts close together
- Itching or discomfort in your genital area
- Bleeding with intercourse
Complications
HPV infection complications can include:
- Cancer. Cervical cancer has been closely linked with genital HPV infection. Certain types of HPV also are associated with cancers of the vulva, anus, penis, and mouth and throat.
- HPV infection doesn’t always lead to cancer, but it’s important for women to have regular Pap tests, particularly those who’ve been infected with higher risk types of HPV.
- Problems during pregnancy. Rarely during pregnancy, warts can enlarge, making it difficult to urinate. Warts on the vaginal wall can inhibit the stretching of vaginal tissues during childbirth.
- Large warts on the vulva or in the vagina can bleed when stretched during delivery.
Extremely rarely, a baby born to a mother with genital warts develops warts in the throat. The baby might need surgery to keep the airway from being blocked.

When to see a doctor
See a doctor if you or your partner develops bumps or warts in the genital area.
How are genital warts diagnosed?
To diagnose this condition, your doctor will do the following:
- Ask questions about your health and sexual history. This includes symptoms you’ve experienced and whether you’ve had sex, including oral sex, without condoms or oral dams.
- Your doctor may perform the following tests to check for genital warts and/or related STDs
- An examination of visible growths to see if they look like genital warts
- Application of a mild acetic acid (vinegar) solution to highlight less visible growths
- Pap Tests
- Pap testOpen pop-up dialog box
- For women, it’s important to have regular pelvic exams and Pap tests, which can help detect vaginal and cervical changes caused by genital warts or the early signs of cervical cancer.
- During a Pap test, your doctor uses a device called a speculum to hold open your vagina and see the passage between your vagina and your uterus (cervix). He or she will then use a long-handled tool to collect a small sample of cells from the cervix. The cells are examined with a microscope for abnormalities.
- A complete pelvic exam and Pap smear (for women)
- Biopsy of cervical tissue ( if abnormal pap smear or visible abnormality) to make sure there are no abnormal cells that could develop into HPV-related cervical cancer; a cervical biopsy involves taking a small sample of tissue from the cervix and examining it under a microscope.
- A specialized test for high-risk HPV (low risk should not be screened for), collected in a way similar to a Pap smear
- HPV Test
- Only a few types of genital HPV have been linked to cervical cancer. A sample of cervical cells, taken during a Pap test, can be tested for these cancer-causing HPV strains.
- This test is generally reserved for women age 30 and older. It isn’t as useful for younger women because for them, HPV usually goes away without treatment.
- Examination of the rectum
- Female patients may be referred to a gynecologist (a doctor who specializes in female reproductive health) for further testing and biopsy.
How is Genital Warts treated?
Treatments can remove genital warts, but they may return.
There is no cure for the infection that causes them, but the body may clear the infection over time.
People should not apply treatments designed to eliminate warts on the hands or feet to their genitals.
Genital wart outbreaks usually resolve without treatment. However, in some cases, the warts grow or multiply without intervention. Also, treating outbreaks of these warts can greatly reduce the risk of transmission.
If your warts aren’t causing discomfort, you might not need treatment. But if you have itching, burning and pain, or if you’re concerned about spreading the infection, your doctor can help you clear an outbreak with medications or surgery.
Medications
Genital wart treatments that can be applied directly to your skin include:
- Imiquimod (Aldara, Zyclara). This cream appears to boost your immune system’s ability to fight genital warts. Avoid sexual contact while the cream is on your skin. It might weaken condoms and diaphragms and irritate your partner’s skin. One possible side effect is skin redness. Other side effects might include blisters, body aches or pain, a cough, rashes, and fatigue.
- Podophyllin and podofilox (Condylox). Podophyllin is a plant-based resin that destroys genital wart tissue. Your doctor applies this solution. Podofilox contains the same active compound, but you can apply it at home. Never apply podofilox internally. Additionally, this medication isn’t recommended for use during pregnancy. Side effects can include mild skin irritation, sores or pain.
- Trichloroacetic acid. This chemical treatment burns off genital warts, and can be used for internal warts. Side effects can include mild skin irritation, sores or pain.
- Sinecatechins (Veregen). This cream is used for treatment of external genital warts and warts in or around the anal canal. Side effects, such as reddening of the skin, itching or burning, and pain, are often mild. Don’t try to treat genital warts with over-the-counter wart removers. These medications aren’t intended for use in the genital area.
Surgery
You might need surgery to remove larger warts, warts that don’t respond to medications or, if you’re pregnant, warts that your baby can be exposed to during delivery. Surgical options include:
- Freezing with liquid nitrogen (cryotherapy). Freezing works by causing a blister to form around your wart. As your skin heals, the lesions slough off, allowing new skin to appear. You might need to repeat the treatment. The main side effects include pain and swelling.
- Electrocautery. This procedure uses an electrical current to burn off warts. You might have some pain and swelling after the procedure.
- Surgical excision. Your doctor might use special tools to cut off warts. You’ll need local or general anesthesia for this treatment, and you might have pain afterward.
- Laser treatments. This approach, which uses an intense beam of light, can be expensive and is usually reserved for extensive and tough-to-treat warts. Side effects can include scarring and pain.
How to prevent Genital Warts
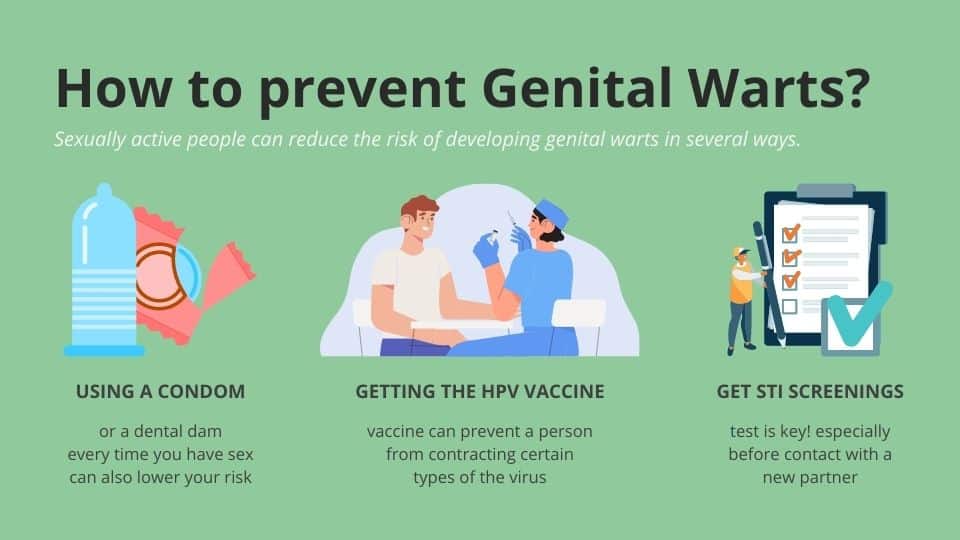
Sexually active people can reduce the risk of developing genital warts in several ways.
- Using a condom or a dental dam every time you have sex can also lower your risk of contracting genital warts. The important thing is to use a physical barrier to prevent transmission.
- Getting the HPV vaccine can prevent a person from contracting certain types of the virus including those that can cause genital warts or cancer.
- Gardasil and Gardasil 9 can protect people of all genders from the most common HPV strains that cause genital warts, and can also protect against strains of HPV that are linked to cervical cancer.
- People from ages 9 to 45 can receive these vaccines. They’re administered in a series of two or three shots, depending on age. Both types of vaccine should be given before the person becomes sexually active, as they’re most effective before a person is exposed to HPV.
- It is important for sexually active people to keep in mind that a person can transmit HPV without knowing that they have it — without the presence of genital warts.
- Having regular STI screenings is key, especially before contact with a new partner.
How Long Do Genital Warts Last?
How long genital warts last can vary from person to person. Sometimes, the immune system clears the warts within a few months. But even if the warts go away, the HPV might still be active in the body. So the warts can come back. Usually within 2 years, the warts and the HPV are gone from the body.
When Is Someone With Genital Warts No Longer Contagious?
People with genital warts definitely can spread HPV. But even after the warts are gone, HPV might still be active in the body. That means it can spread to someone else through sex or close sexual contact and cause warts in that person. It’s hard to know when people are no longer contagious, because there’s no blood test that looks for HPV.
References
What to know about genital warts
- medicalnewstoday.com/articles/155236#what-are-they
Genital Warts
- healthline.com/health/std/genital-warts
Genital warts
- mayoclinic.org/diseases-conditions/genital-warts/diagnosis-treatment/drc-20355240
Genital Warts (HPV)
- kidshealth.org/en/teens/std-warts.html
Genital Warts and HPV
- webmd.com/sexual-conditions/hpv-genital-warts/genital-warts#091e9c5e80011c99-1-4
