HIV is one of the chronic infectious diseases that requires continuous antiretroviral therapy (ART) to control the viral load in the body. However, recent research has revealed a significant breakthrough that could change the future approach to HIV treatment. A new study has found that some people living with HIV can stop taking ART for up to nearly one year after receiving injections of two types of antibodies. This may mark the first step toward developing HIV treatments that reduce reliance on daily antiretroviral medication.

A Study That Could Change HIV Treatment Approaches For People Living with HIV
What is the RIO trial?
RIO (Research in Immunotherapy and Outcomes) is a research study conducted in the United Kingdom and Denmark, aimed at evaluating whether the use of two types of antibodies can help people living with HIV stop taking antiretroviral therapy (ART) for an extended period of time.
Objective of the Trial
The aim of this trial is to test whether people living with HIV can control the amount of virus in their body without the need for ART, by using Broadly Neutralizing Antibodies (bNAbs) — antibodies that can broadly prevent and fight against the HIV virus.
Trial Details
- Number of participants: 68 people
- Study design: Randomized Controlled Trial (RCT)
- Participants: People living with HIV who were on ART and had successfully suppressed their viral load to low levels.
- Types of antibodies used:
- 3BNC117 – An antibody that binds to the HIV envelope protein and prevents the virus from entering cells.
- 10-1074 – An antibody that targets the V3 loop of the HIV envelope protein and helps block the virus from spreading.
Trial Process
- All participants were divided into two groups:
- First group: Received the 3BNC117 and 10-1074 antibodies.
- Second group: Received a placebo.
- All participants were asked to stop taking ART and were closely monitored to track their viral levels.
- The research team observed how long each participant could control the virus without needing to resume ART.
RIO Trial Results
- During the first 20 weeks:
- In the placebo group, only 3 out of 31 participants (9%) were able to remain off ART without viral rebound.
- In the antibody group, 12 out of 34 participants (35%) successfully controlled the virus without resuming ART.
- At week 48 (nearly 1 year):
- 57% of those who received the antibodies were still able to control the virus without ART.
- At week 72 (around 1.5 years):
- 39% of the participants who received the antibodies still had viral loads under 1,000 copies/ml.
- Remarkably, 7 individuals showed no viral rebound at all for almost 2 years after stopping ART.
The Importance of the RIO Trial for People Living with HIV
- This is the first evidence showing that antibodies may help people with HIV stop ART for an extended period.
- It could be the first step toward developing HIV treatment strategies that do not rely on daily antiretroviral medication.
- The results indicate that antibody therapy may offer a new, long-term HIV control approach.
Limitations of the Trial
- The study is still small in scale — larger trials are needed.
- Results vary between individuals — while some were able to stop ART for up to 2 years, others needed to restart treatment sooner.
- Risk of resistance — in some cases, HIV may develop resistance to the antibodies.
- High cost — antibody production remains expensive, limiting accessibility for most patients.
How Antibodies Work in HIV Treatment
“The antibodies used in this study are broadly neutralizing antibodies (bNAbs), which are highly effective at targeting and neutralizing the HIV virus. They work in two ways:
- 3BNC117 — binds to the HIV envelope protein and prevents the virus from entering T cells.
- 10-1074 — blocks the spread of the virus within the body by targeting the V3 loop of the envelope protein.
The combination of these two antibodies allows the immune system to clear the virus more effectively, which may explain why patients were able to control their viral load for longer periods without the need for ART.”
The Potential of Antibodies as a Treatment for People Living with HIV
How it differs from traditional ART
Traditional ART works by suppressing the replication of the virus but does not enable the body to control the virus on its own. In contrast, the use of long-acting antibodies may help patients reduce their reliance on daily ART, with the possibility of controlling the virus without needing daily medication in the future.
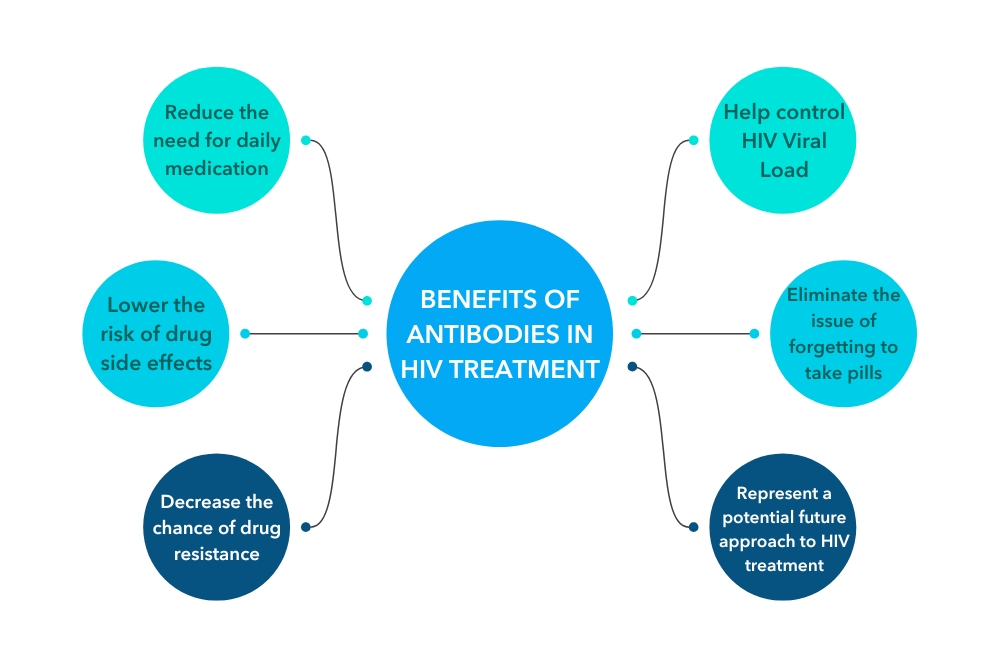
Benefits of Using Antibodies in HIV Treatment
The use of antibodies (Broadly Neutralizing Antibodies — bNAbs) for HIV treatment is gaining attention, as they may help people living with HIV control the virus without relying on daily antiretroviral therapy (ART).
1. Reducing the burden of daily ART
Most people living with HIV need to take ART every day to keep the virus under control. However, long-acting antibodies can reduce the frequency of treatment, improving patients’ quality of life. The RIO trial found that 57% of participants were able to stop ART for nearly one year after receiving antibodies — a promising sign for developing HIV treatments that don’t require daily medication.
2. Helping the immune system control the virus more effectively
Antibodies can enhance the body’s ability to respond to HIV without the need for constant ART. While ART only suppresses viral replication, antibodies like 3BNC117 and 10-1074 can actively destroy the virus and help the body build its own defense mechanisms.
3. Reducing the risk of long-term ART side effects
Long-term ART use can lead to side effects such as:
- Nausea and dizziness
- Liver and kidney problems
- Abnormal blood lipid levels
- Increased risk of heart disease
Long-acting antibody injections can reduce the need for daily ART, sparing patients from these long-term side effects.
4. Making HIV treatment more convenient
Some HIV patients struggle with daily medication due to:
- Forgetting to take ART regularly
- Mental health challenges around taking medication
- Wanting to keep their HIV status private
Long-acting antibodies that may only need to be administered a few times a year make treatment more convenient and reduce the stress of daily adherence.
5. Lowering the risk of ART resistance
One of the major problems with long-term ART use is the risk of the virus developing drug resistance, which can make treatment ineffective. Antibodies have the potential to reduce this risk, as they target various proteins on HIV, making it harder for the virus to develop resistance.
6. A possible first step toward an HIV cure
Current ART cannot eliminate HIV from the body, but antibody-based therapy may help the body control the virus without ongoing medication. This could be an important step toward the development of a functional cure for HIV in the future.
Challenges and Limitations of Using Antibodies
Although this study marks a significant step forward in the field of HIV research, there are still several obstacles to consider:
| ✦ Different patient responses | ▶︎ Not everyone can remain off ART for extended periods. |
| ✦ High cost of antibodies | ▶︎ Antibody production remains expensive, limiting widespread accessibility. |
| ✦ Risk of resistance | ▶︎ HIV can develop resistance to antibodies in some cases. |
| ✦ Need for periodic injections | ▶︎ While daily ART may not be necessary, patients will still need to receive regular antibody injections. |
Future Directions for HIV Treatment
Researchers are exploring new approaches to HIV treatment, including:
- Developing longer-acting antibodies to reduce the frequency of injections
- Combining antibody therapy with T-cell therapies (such as CAR-T cell therapy)
- Using gene therapy to eliminate HIV from the body
- Developing therapeutic HIV vaccines to create long-lasting immunity

FAQ About Antiretroviral Therapy (ART)
☞ ART (Antiretroviral Therapy) is the use of antiretroviral medications to control HIV in the body. These medications help reduce the viral load in the blood to an undetectable level, strengthening the immune system and preventing the transmission of HIV to others.
☞ No, ART cannot cure HIV. However, it can suppress the virus to undetectable levels, allowing people living with HIV to live long, healthy lives just like anyone else.
☞ Yes. Currently, there is no cure for HIV. Stopping ART can cause the virus to rebound and increases the risk of developing drug resistance. However, new research is exploring the possibility of taking breaks from medication in the future.
☞ Some people may experience side effects such as nausea, dizziness, fatigue, or vivid dreams, especially during the first few weeks as the body adjusts. In some cases, long-term side effects can occur, such as liver or kidney problems, so regular health check-ups are recommended.
☞ If you forget to take your medication and remember within 12 hours, take it as soon as you can. But if it’s close to your next scheduled dose, skip the missed one and continue as normal. Do not double the dose, as this can lead to side effects or drug resistance.
☞ If you take ART consistently and achieve an undetectable viral load (U=U: Undetectable = Untransmittable), you cannot transmit HIV through sex. However, condoms are still recommended to protect against other sexually transmitted infections (STIs), such as syphilis, gonorrhea, and hepatitis.
Related Articles
- HIV and Mental Health : Understanding the Connection and Coping Strategies
- Innovations in HIV Medication – A Path Towards a Cure
In Summary The recent discovery of using antibodies to control HIV without daily ART could be a major milestone in transforming the future of HIV treatment. The study found that some patients were able to stop ART for nearly one year, which could lead to the development of new treatment methods that reduce the burden of continuous medication.
However, there are still challenges and limitations that must be addressed before this approach can become a widely adopted standard of care. Researchers will need to conduct further studies to develop antibodies that are even more effective and safe.
“In the future, we may witness a new era of HIV treatment — one that no longer relies on daily medication and offers people living with HIV the opportunity to control the virus more effectively.”
Reference:
การทดลองทางคลินิกเกี่ยวกับ HIV และ AIDS
- hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-and-aids-clinical-trials
การวิจัยการรักษา HIV ในปี 2024
- healthequitymatters.org.au/resources/hiv-cure-research-in-2024
การรักษาด้วยยาต้านไวรัส (แอนไทเรโทรไวรัล. ทีราพี, เออาร์ที)
- fpnsw.org.au/sites/default/files/assets/thai_treatments.pdf
Last Updated on 18/03/2025 by ทีมที่ปรึกษา มูลนิธิเพื่อรัก

