PrEP and PEP for HIV prevention. These treatments are proven effective in preventing HIV transmission In turn, while both have similar objectives, the differences in PrEP vs. PEP for HIV prevention depend on the individual and whether or not they’ve already been exposed.
PrEP and PEP are medicines to prevent HIV. Each type is used in a different situation:
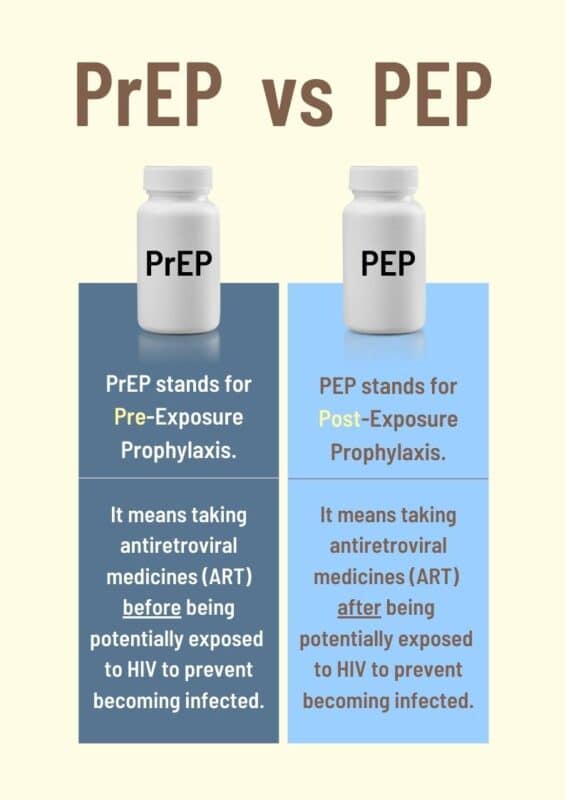
PrEP stands for pre-exposure prophylaxis. It is for people who don’t already have HIV but are at very high risk of getting it. PrEP is daily medicine that can reduce this risk. With PrEP, if you do get exposed to HIV, the medicine can stop HIV from taking hold and spreading throughout your body.
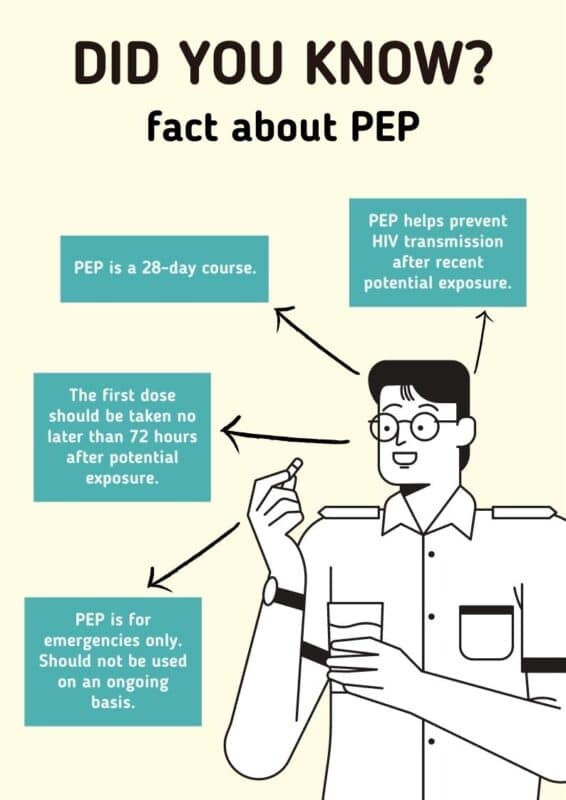
PEP stands for post-exposure prophylaxis. PEP is for people who have possibly been exposed to HIV. It is only for emergency situations. PEP must be started within 72 hours after a possible exposure to HIV.

Difference between PrEP and PEP
- PrEP = pre-exposure prophylaxis.
- As indicated by ‘pre’, you start to take it before you may be exposed to HIV.
- PrEP is designed to be used in a planned way, on an ongoing basis.
- Most people take PrEP once a day, every day. Some people can use ‘event-based’ dosing, which involves taking it before sex and then for two days afterwards.
- There are two drugs in PrEP. They are usually combined in a single tablet.
- PEP = post-exposure prophylaxis.
- As indicated by ‘post’, you start to take it after a single event that may have exposed you to HIV.
- PEP is used in emergency situations.
- PEP is a four-week course of drugs, taken once a day during that time. It is best to start PEP within 24 hours of exposure to HIV, but certainly within 72 hours.
- There are three drugs in PEP – usually the same two that are taken for PrEP, plus a third one. They are usually provided in two tablets.
Who are they for
PrEP : People without HIV who have
- Had condomiess sex with a partner with HIV
- Had condomiess sex with a partner of unknow HIV status
- Shared needles
PEP : People without HIV who have
- Had condomiess sex with a partner of unknow HIV status
- Shared needles
- Had a workplace injury
- Experienced sexual assault
Who should consider taking PrEP?
PrEP is for people without HIV who are at very high risk for getting it. This includes:
Gay/bisexual men who:
- Have an HIV-positive partner
- Have multiple partners, a partner with multiple partners, or a partner whose HIV status is unknown and
- Have anal sex without a condom OR
- Have been diagnosed with a sexually transmitted disease (STD) in the last 6 months
Heterosexual men and women who:
- Have an HIV-positive partner
- Have multiple partners, a partner with multiple partners, or a partner whose HIV status is unknown and
- Don’t always use a condom when having sex with people who inject drugs OR
- Don’t always use a condom when having sex with bisexual men
People who inject drugs and:
- Share needles or other equipment to inject drugs OR
- Are at risk for getting HIV from sex
- If you have a partner who is HIV-positive and are considering getting pregnant, talk to your health care provider about PrEP. Taking it may help protect you and your baby from getting HIV infection while you try to get pregnant, during pregnancy, or while breastfeeding.’
Who should consider taking PEP?
- If you are HIV-negative and you think you may have been recently exposed to HIV, contact your health care provider immediately or go to an emergency room right away.
- You may be prescribed PEP if you are HIV negative or don’t know your HIV status, and in the last 72 hours you:
- Think you may have been exposed to HIV during sex,
- Shared needles or drug preparation equipment, OR
- Were sexually assaulted
- Your health care provider or emergency room doctor will help to decide whether PEP is right for you.
- PEP may also be given to a health care worker after a possible exposure to HIV at work, for example, from a needlestick injury.
PrEP and PEP Are they effective?
PrEP
Daily PrEP can reduce the risk of HIV transmission from sex by more than 90% and from shared needles by more than 70%
PEP
When taken correctly, PEP can reduce the risk of HIV transmission by almost 80% It’s still important to use condoms, other barrier methods, and cautious injection practices
Are They safe?
PrEP Side Effects
Common side effects from taking the PrEP medication include a slight increase in bowel movements, an upset stomach, headaches, and dry mouth.However, those side effects usually subside within two to four weeks. If side effects continue any longe
PEP Side Effects
PEP side effects are similar to PrEP side effects, as in you might experience gastrointestinal issues, headaches, or changes in your sleep patterns. However, these side effects tend to subside within the first few days of taking the medication and definitely by two weeks. Since the treatment is only 28 days, mild side effects are usually bearable for patients who are worried about HIV exposure.

Where can people get them?
PrEP :
The National Health Security Office (NHSO) has introduced a groundbreaking benefit for Thai citizens by incorporating Pre-Exposure Prophylaxis (PrEP) for HIV prevention into the services covered under the national health security system. This initiative represents a pivotal step in curbing the spread of HIV in Thailand while ensuring greater access to essential healthcare services, particularly for high-risk groups.
In Thailand, PrEP is widely available and can be accessed through various healthcare providers, clinics, and organizations. Here are some key options:
- Provincial Hospitals: Many government hospitals in major cities and provinces provide PrEP services.
- Non-Governmental Organizations (NGOs): NGOs play a vital role in offering PrEP and related support services.
- Private Clinics: Private healthcare facilities also offer PrEP for those seeking alternative service providers.
This comprehensive availability ensures individuals across Thailand have the opportunity to access PrEP based on their preferences and needs. or you can book via Love2test service for free here!
Note : An HIV test is required before starting PrEP and every 3 months during PrEP treatment
PEP : Via prescription from a healthcare provider or emergency room doctor
PrEP and PEP Medications Available
Cost of PrEP
Most health insurance plans, including Medicaid, cover PrEP. Check with your insurance company to see if PrEP is covered on your plan. If you don’t have health insurance, you can still get help paying for PrEP. has a medication assistance program that could make PrEP free for you. The staff at your local health center can also help you apply for health insurance or assistance programs that can make PrEP affordable or free for you
Cost of PEP
The process of getting PEP treatments covered is similar to PrEP. Make sure that when you go to get your PEP treatment, you go to an experienced provider, HIV specialist, or urgent care clinic that understands the urgency of getting this treatment to you. You shouldn’t face barriers to access, as you need to take the treatment within that 72-hour window of exposure. Your health care provider can apply for free PEP medicines through the medication assistance programs run by the manufacturers.
References for PrEP and PEP
HIV: PrEP and PEP
- medlineplus.gov/hivprepandpep.html
PrEP vs. PEP: What Do They Do?
- healthline.com/health/hiv-aids/hiv-prevention/prep-vs-pep-infographic#infographic
What’s the difference between PrEP and PEP for HIV prevention?
- aidsmap.com/about-hiv/whats-difference-between-prep-and-pep-hiv-prevention
Difference Between PrEP vs. PEP for HIV Prevention
- erineverettnp.com/articles/2020/09/23/prep-vs-pep-hiv-prevent