Hepatitis C is inflammation of the liver. Inflammation is swelling that happens when tissues of the body are injured or infected. Inflammation can damage organs.
There are different types of hepatitis. One type, hepatitis C, is caused by the hepatitis C virus (HCV). Hepatitis-C Virus can range from a mild illness lasting a few weeks to a serious, lifelong illness. The virus spreads through an infected person’s blood or body fluids.
List of contents
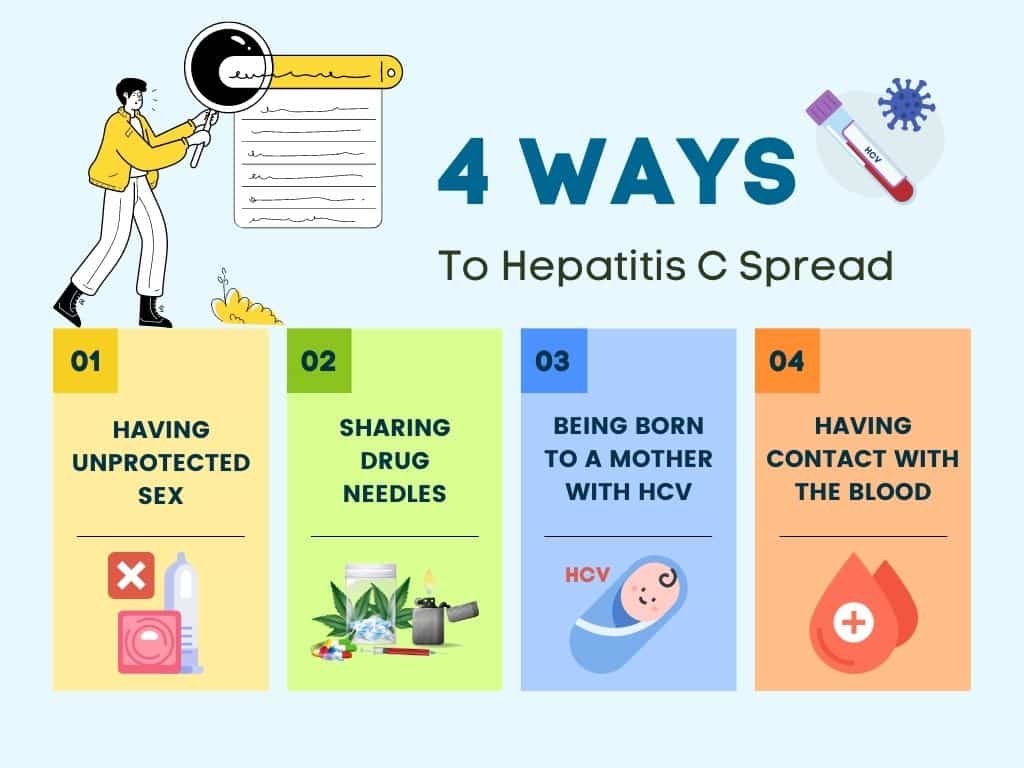

How is hepatitis C spread?
Hepatitis C spreads through contact with the blood of someone who has HCV. This contact may be through:
- Sharing drug needles or other drug materials with someone who has HCV.
- Being tattooed or pierced with tools or inks that were not sterilized after being used on someone who has HCV
- Having contact with the blood or open sores of someone who has HCV
- Sharing personal care items that may have come in contact with another person’s blood, such as razors or toothbrushes
- Being born to a mother with HCV
- Having unprotected sex with someone who has HCV
Stages of Hepatitis C
The hepatitis C virus affects people in different ways and has several stages:
Incubation period. This is the time between first exposure to the start of the disease. It can last anywhere from 14 to 80 days, but the average is 45
Acute hepatitis C.
This is a short-term illness that lasts for the first 6 months after the virus enters your body. After that, some people who have it will get rid of, or clear, the virus on their own.
Chronic hepatitis C.
For most people who get hepatitis C — up to 85% — the illness moves into a long-lasting stage (longer than 6 months). This is called a chronic hepatitis C infection and can lead to serious health problems like liver cancer or cirrhosis.
Cirrhosis.
This disease leads to inflammation that, over time, replaces your healthy liver cells with scar tissue. It usually takes about 20 to 30 years for this to happen, though it can be faster if you drink alcohol or have HIV.
Liver cancer.
Cirrhosis makes liver cancer more likely. Your doctor will make sure you get regular tests because there are usually no symptoms in the early stages.
Who is at risk?
You are more likely to get hepatitis C if you:
- Have injected drugs
- Had a blood transfusion or organ transplant before July 1992
- Have hemophilia and received clotting factor before 1987
- Have been on kidney dialysis
- Were born between 1945 and 1965
- Have abnormal liver tests or liver disease
- Have been in contact with blood or infected needles at work
- Have had tattoos or body piercings
- Have worked or lived in a prison
- Were born to a mother with HCV
- Have HIV/AIDS
- Have had more than one sex partner in the last 6 months
- Have had a sexually transmitted disease
- Are a man who has had sex with men
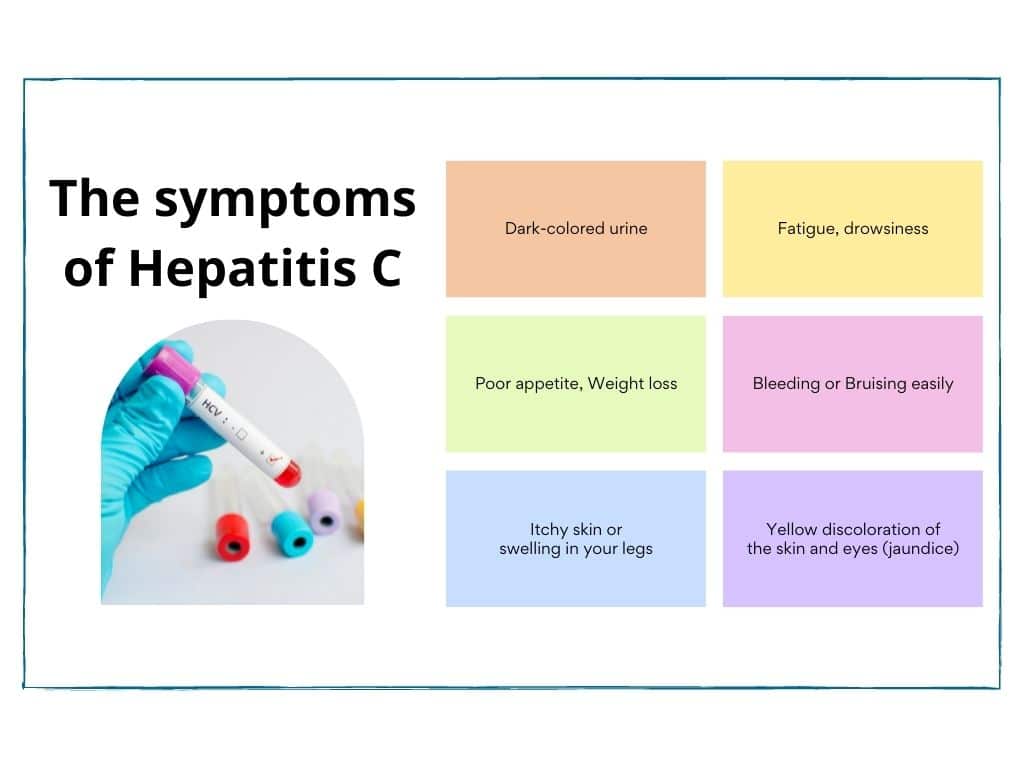
What are the symptoms of hepatitis C?
Long-term infection with the hepatitis C virus is known as chronic HCV. Chronic hepatitis C is usually a “silent” infection for many years, until the virus damages the liver enough to cause the signs and symptoms of liver disease.
Signs and symptoms include:
- Bleeding easily
- Bruising easily
- Fatigue
- Poor appetite
- Yellow discoloration of the skin and eyes (jaundice)
- Dark-colored urine
- Itchy skin
- Fluid buildup in your abdomen (ascites)
- Swelling in your legs
- Weight loss
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
- Spiderlike blood vessels on your skin (spider angiomas)
Acute hepatitis C
infection doesn’t always become chronic. Some people clear HCV from their bodies after the acute phase, an outcome known as spontaneous viral clearance. In studies of people diagnosed with acute HCV, rates of spontaneous viral clearance have varied from 15% to 25%. Acute HCV also responds well to antiviral therapy.
Every chronic hepatitis C
infection starts with an acute phase. Acute HCV usually goes undiagnosed because it rarely causes symptoms. When signs and symptoms are present, they may include jaundice, along with fatigue, nausea, fever and muscle aches. Acute symptoms appear one to three months after exposure to the virus and last two weeks to three months.
Possible Complications
There’s one main complication of acute hepatitis C: It could become chronic.
If you go on to develop chronic hepatitis C, you could eventually experience a number of health complications, including:
- Cirrhosis, or scarring of the liver. With cirrhosis, scar tissue gradually replaces healthy tissue in your liver, blocking blood flow and disrupting liver function. Cirrhosis can eventually lead to liver failure.
- Liver cancer. Having chronic HCV raises your risk for eventually developing liver cancer. If you develop cirrhosis or your liver is very damaged before treatment, you’ll still have a higher risk for cancer after getting treated.
- Liver (hepatic) failure. It takes a long time for your liver to fail. Liver failure, or end-stage liver disease, happens slowly over months, often years. When your liver becomes unable to function properly, you’ll need a transplant.
If you believe you contracted the HCV, a good next step involves reaching out to a healthcare professional. Getting timely treatment can lower your risk for experiencing serious complications.
Hepatitis C Testing and Diagnosis
Doctors will start by checking your blood for:
- Blood tests. They may order a series of blood tests to check for the virus, starting with a hepatitis C antibody test. A PCR test can tell your healthcare professional whether the virus is currently active, and viral load testing can measure the amount of virus in your blood.
- Genotype test. This test can reveal which hepatitis C genotype you have. This information will help your healthcare professional find an effective treatment approach.
- Liver biopsy. This procedure can also help check for liver damage. A biopsy involves taking a small piece of tissue from your liver and testing it for cell abnormalities.
- Anti-HCV antibodies: These are proteins your body makes when it finds the hep C virus in your blood. They usually show up about 12 weeks after infection.
It usually takes a few days to a week to get results, though a rapid test is available in some places.
The results can be:
- Nonreactive, or negative:
- That may mean you don’t have hep C.
- If you’ve been exposed in the last 6 months, you’ll need to be retested.
- Reactive, or positive:
- That means you have hep C antibodies and you’ve been infected at some point.
- You’ll need another test to make sure.
If your antibody test is positive, you’ll get this test:
HCV RNA: It measures the number of viral RNA (genetic material from the hepatitis virus) particles in your blood. They usually show up 1-2 weeks after you’re infected. The results can be:
- Negative: You don’t have hep C.
- Positive: You currently have hep C.
You might also get:
Liver function tests: They measure proteins and enzyme levels, which usually rise 7 to 8 weeks after you’re infected. As your liver gets damaged, enzymes leak into your bloodstream. But you can have normal enzyme levels and still have HCV. Learn the reasons why you should get tested for hepatitis C.
Treatment and Medication
If you have acute HCV, there is no recommended treatment. If your HCV turns into a chronic hepatitis C infection, there are several medications available.
Interferon, peginterferon, and ribavirin used to be the main treatments for HCV. They can have side effects like fatigue, flu-like symptoms, anemia, skin rash, mild anxiety, depression, nausea, and diarrhea.
Now you’re more likely to get one of these medications:
- Elbasvir-grazoprevir (Zepatier). This once-daily pill has cured the disease in as many as 97% of those treated.
- Glecaprevir-pibrentasvir (Mavyret). This daily pill offers a shorter treatment cycle of 8 weeks for adult patients with all types of HCV who don’t have cirrhosis and who haven’t already been treated. The treatment is longer for those who are in a different disease stage. The prescribed dosage for this medicine is 3 tablets daily.
- Ledipasvir-sofosbuvir (Harvoni). This once-daily pill cures the disease in most people in 8-12 weeks.
- Ombitasvir-paritaprevir-dasabuvir-ritonavir (Viekira Pak). This treatment is a combo of pills: two that you’ll take once a day, and one you’ll take twice with meals. You’ll take it for 12 to 24 weeks.
- Ombitasvir-paritaprevir- ritonavir (Technivie). You’ll take this tablet by mouth, possibly along with ribavirin.
- Sofosbuvir (Sovaldi) with elbasvir/grazoprevir. Take this tablet at the same time every day with food. You have to take it along with ribavirin and/or interferon, and you’ll probably be on it for 12 to 24 weeks.
- Sofosbuvir-velpatasvir (Epclusa). This daily pill, which you typically take for 12 weeks, should cure your disease.
- Sofosbuvir-velpatasvir-voxilaprevir (Vosevi). This combination is approved to treat adults with chronic HCV, either with no cirrhosis or with compensated cirrhosis (the stage of the disease that doesn’t have symptoms), who’ve already had certain treatments.
Can Hepatitis C be cured?
Yes. Modern treatments can cure hepatitis C in most cases. These treatments involve a combination of antiviral medications taken for 8–24 weeksTrusted Source. However, as many people with HCV do not know they are infected, they may not seek testing and treatment for many years.
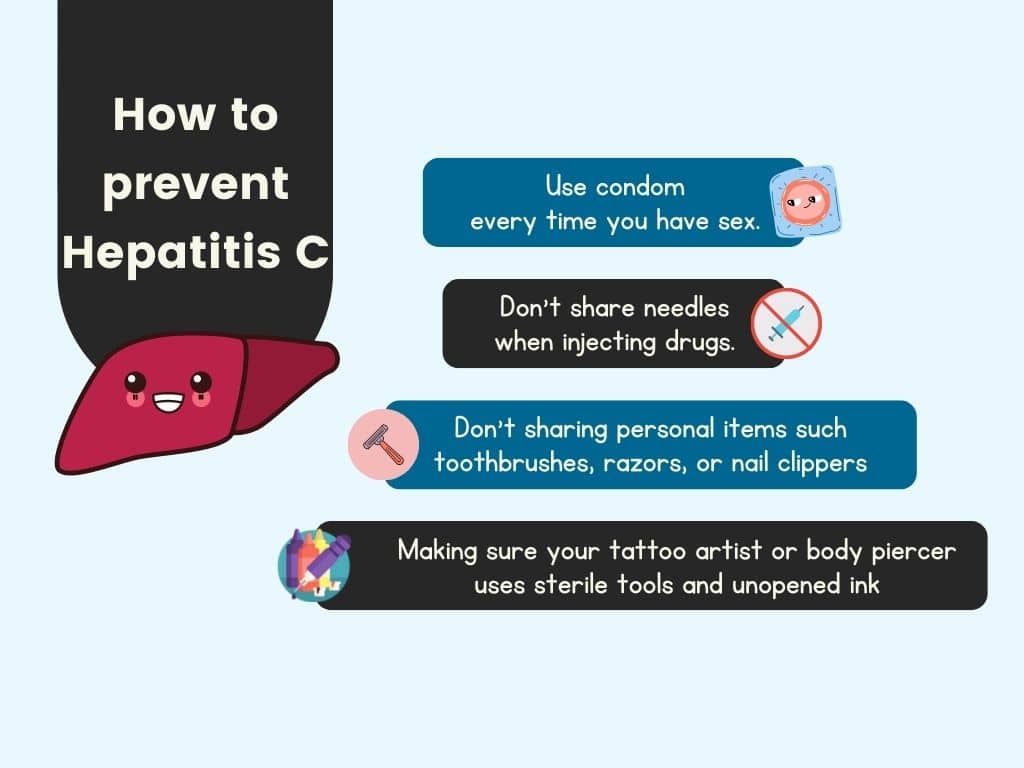
How to prevent?
Protect yourself from HCV infection by taking the following precautions:
- Use a latex condom every time you have sex.
- Don’t share needles, syringes, or other equipment when injecting drugs.
- Wearing gloves if you have to touch another person’s blood or open sores
- Making sure your tattoo artist or body piercer uses sterile tools and unopened ink
- Not sharing personal items such toothbrushes, razors, or nail clippers
References
Hepatitis C
- mayoclinic.org/diseases-conditions/hepatitis-c/symptoms-causes/syc-20354278
Hepatitis C and the Hep C Virus
- webmd.com/hepatitis/digestive-diseases-hepatitis-c
Hepatitis C
- medlineplus.gov/hepatitisc.html
Everything You Want to Know About Hepatitis C
- healthline.com/health/hepatitis-c#symptoms-in-men
What to know about hepatitis C
- medicalnewstoday.com/articles/294705

