Many people have probably heard about medications used to prevent HIV infection, such as PrEP and PEP. However, there are still many misunderstandings about how these medicines work. Some people take the wrong type, use them incorrectly, or believe they can simply buy PrEP or PEP over the counter at any pharmacy. In reality, these HIV prevention drugs must be prescribed by a doctor after consultation and blood testing. They are considered specialized antiviral medications, and can only be taken if you are HIV-negative at the time of screening.
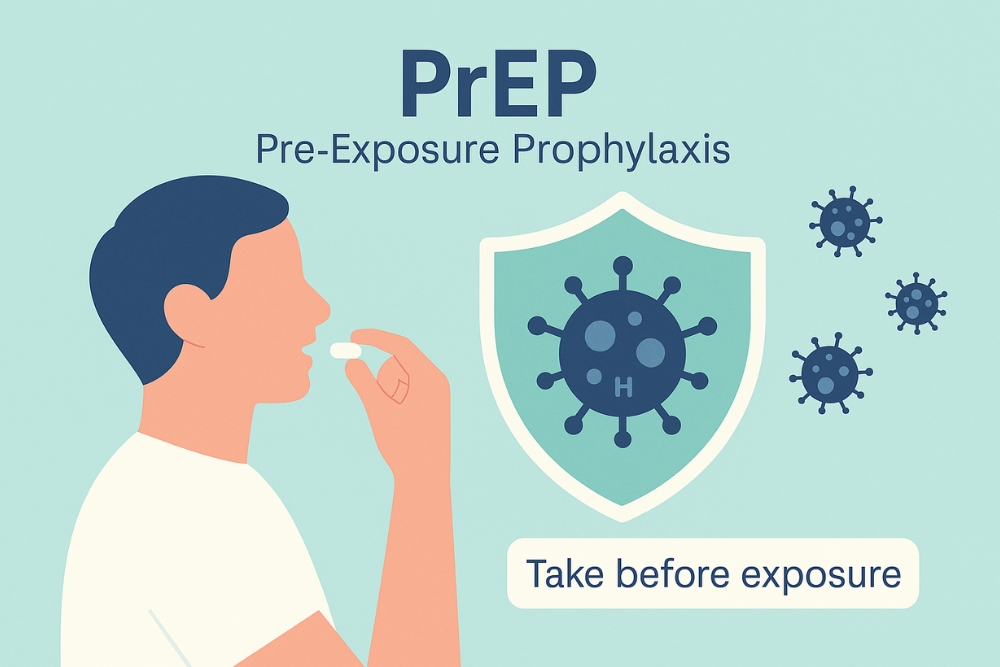
What is PrEP?
PrEP (Pre-Exposure Prophylaxis) is a medication used to prevent HIV infection before potential exposure — in simple terms, before having sex. When taken consistently in sufficient amounts, PrEP helps block the virus from multiplying inside the body.
Before starting PrEP, you must consult a doctor and undergo several health checks to ensure you’re ready for the medication, including:

- HIV testing
- Liver function tests
- Kidney function tests
- Hepatitis B screening
- STIs testing
- Pregnancy test (for women)
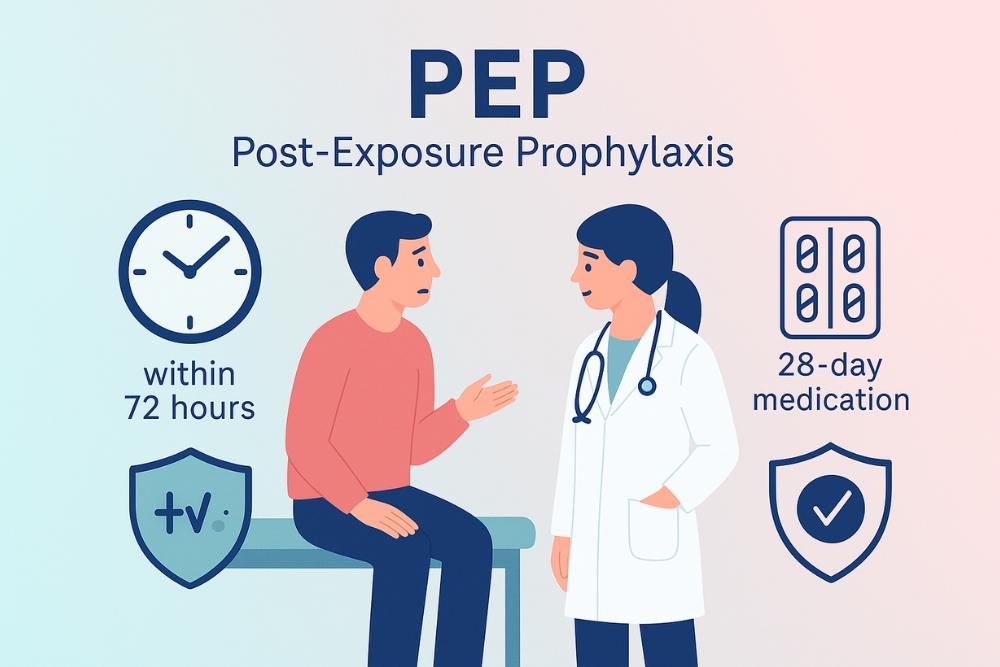
What is PEP?
PEP (Post-Exposure Prophylaxis) is a medication taken after potential exposure to HIV — for instance, after having sex with someone who might be HIV-positive. PEP works by stopping the virus from replicating and becoming established in the body, allowing your immune system to eliminate it before infection occurs.
Before prescribing PEP, a doctor will assess your risk and confirm you don’t already have HIV. Common tests include:
- HIV testing
- Liver function (AST, ALT)
- Kidney function (BUN, Cr)
- Hepatitis B surface antigen (HBsAg)
- Hepatitis B antibody (Anti-HBsAg)
- Hepatitis C antibody (Anti-HCV)
- STIs screening
- Pregnancy test (for women)
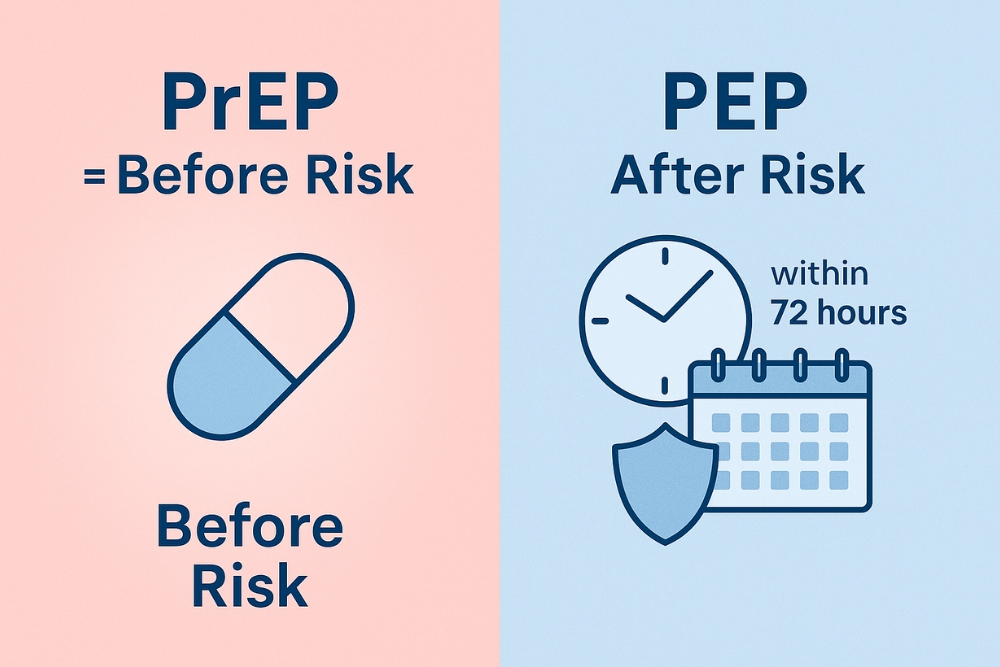
“PrEP is taken before risk; PEP is taken after exposure in an emergency.”
How are PrEP vs PEP different?
In short, PrEP is used before potential HIV exposure, while PEP is used after exposure. If you’re unsure which one is right for you, it’s always best to consult a doctor. Using the wrong medication or taking it incorrectly may reduce its effectiveness and put your health at risk. Doctors will determine the most appropriate option based on your risk level and sexual behavior.
Who should use PrEP vs PEP ?
| PrEP is suitable for | PEP is suitable for |
|---|---|
| People who frequently have sex without condoms | Those who had sex without a condom |
| Men who have sex with men | Condom breakage or slippage |
| People with multiple partners or serodiscordant relationships | Victims of sexual assault |
| People who inject drugs | Those who shared injection equipment |
| People diagnosed with an STI within the past 6 months | Those who had unprotected sex while intoxicated |
How to Take PrEP vs PEP
PrEP (Before Exposure)
Take one pill daily at the same time. It should be taken for at least 7 days before potential exposure and continued for 3 months or longer as prescribed. If you miss a dose, take it as soon as you remember — but never double up. When stopping PrEP, continue for 4 weeks after the last sexual encounter, and consult your doctor before discontinuing.
PEP (After Exposure)
PEP should be started as soon as possible — within 72 hours after exposure. The treatment lasts 28 days, and it’s crucial to complete the full course without missing doses. After finishing, return for follow-up HIV testing immediately and again after 3 months. During this period, avoid donating blood and always use condoms.
Do PrEP and PEP Really Prevent HIV?
Both PrEP and PEP are highly effective in preventing HIV infection — PrEP reduces the risk by over 90% when taken correctly, while PEP reduces the risk by 70–80% if started promptly and completed fully. However, neither protects against other STIs such as gonorrhea, syphilis, or herpes. That’s why combining these medications with condom use remains the best strategy for full protection. People taking PrEP should visit their doctor every 3–6 months for HIV testing and health monitoring. Consistent follow-up ensures continued effectiveness and early detection of any side effects or health issues. PEP, meanwhile, is meant for emergencies only — if you find yourself at frequent risk, switching to regular PrEP is more suitable.
Possible Side Effects of PrEP and PEP
Both PrEP and PEP may cause mild, temporary side effects during the first 1–2 weeks, such as headache, nausea, vomiting, or loss of appetite. These usually go away on their own. If symptoms persist beyond two weeks, consult your doctor. When taken correctly under medical supervision, PrEP and PEP are safe and effective tools that can significantly reduce the risk of HIV infection and transmission.
Conclusion
PrEP and PEP are vital tools in modern HIV prevention, empowering individuals to take charge of their own health with confidence. The most important thing is using them correctly under medical supervision — each has a specific purpose and timing. Using the wrong one or skipping doses may reduce their effectiveness. The best HIV prevention comes from a combination of methods: appropriate use of PrEP or PEP, consistent condom use, regular sexual-health checkups, and open communication with your doctor or partner. Being informed and proactive not only protects your health but also helps build a safer, more understanding society for everyone.
References:
↪︎ รู้ไว้! ใช้ PrEP & PEP อย่างถูกวิธี ช่วยลดความเสี่ยงติดเชื้อ HIV

