Liver Diseases, particularly Hepatitis A, B, and C, remain a major health concern that many people in Thailand do not fully understand. Each type has its own mode of transmission, symptoms, severity, and treatment approaches. While they may appear similar at first glance, the actual impact on liver health—and the risks of serious complications such as cirrhosis or liver cancer—are very different.
Understanding these distinctions is essential not only for protecting yourself but also for ensuring timely testing and receiving proper treatment when risks or unusual symptoms occur. This article explores Hepatitis A, B, and C in detail, covering their causes, transmission routes, warning signs, long-term effects, as well as modern approaches to treatment and prevention. With this knowledge, you can better safeguard your liver health and that of your loved ones with confidence.
Liver Diseases – The Silent Threat Affecting Millions of Thais
Hepatitis, one of the most common viral liver diseases, is often called a “silent threat” because it usually shows no clear symptoms in its early stages. Many people may not realize they are infected, as early signs such as fatigue, loss of appetite, or muscle aches are often mistaken for simple exhaustion. Without proper testing, patients may unknowingly allow the disease to progress quietly over time.

In Thailand, Hepatitis B and C are among the most prevalent liver diseases compared to other countries in Asia. These viral infections are leading causes of cirrhosis and liver cancer—serious complications that rank among the top causes of death in the country. Because these viruses can remain hidden in the body for years without obvious symptoms, they are considered especially dangerous. By the time many patients are diagnosed, the disease has already advanced significantly.
Raising awareness about viral liver diseases is therefore essential. Regular liver check-ups, vaccination (particularly for Hepatitis A and B), and continuous treatment for those living with Hepatitis C are crucial strategies to lower the risk of life-threatening complications and to prevent further transmission.
Hepatitis A: Transmission, Symptoms and Treatment
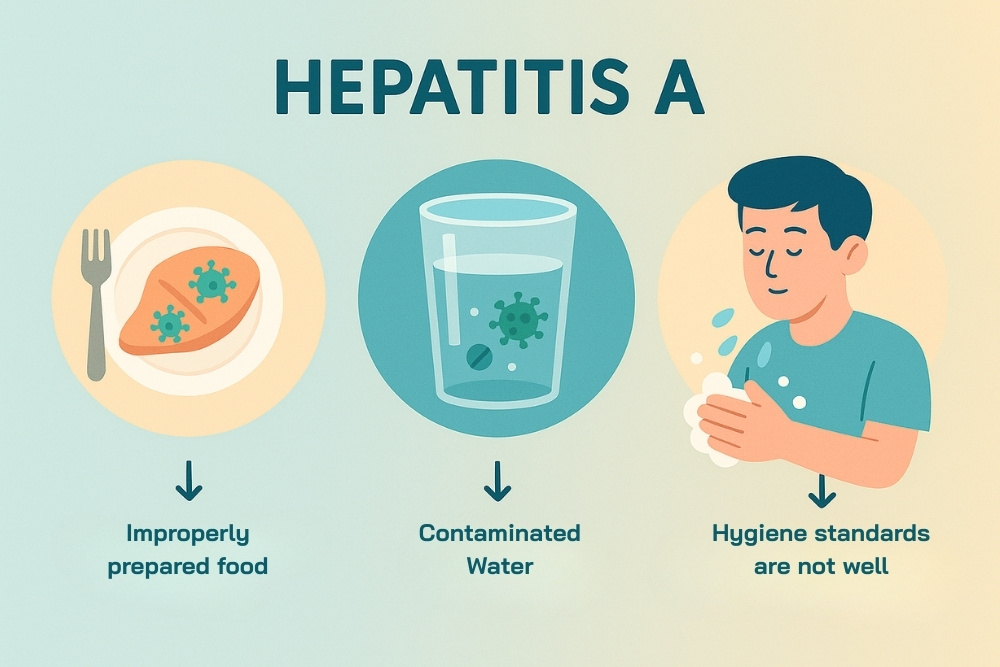
Hepatitis A Virus (HAV) is one of the viral liver diseases that causes inflammation of the liver. What makes it unique is its mode of transmission—primarily through eating and drinking—unlike other types of hepatitis that are commonly spread through blood or sexual contact. Hepatitis A is often found in areas with poor sanitation or among individuals who consume contaminated food and water.
Transmission of Hepatitis A
The virus spreads mainly through the fecal-oral route when contaminated food or water enters the body, or through close contact with an infected person. Sharing utensils or personal items can also spread the virus. Since HAV can survive in the environment for long periods, outbreaks can easily occur in communities where hygiene standards are not well maintained.
Symptoms of Hepatitis A and Related Liver Diseases
Symptoms usually appear 2–6 weeks after infection and may include:
- Fatigue, loss of appetite, nausea and vomiting
- Abdominal pain, especially around the upper right side of the abdomen
- Jaundice (yellowing of the skin and eyes) and dark-colored urine
- In some cases, mild fever and flu-like symptoms
Although these symptoms can cause discomfort, most cases of Hepatitis A are acute and self-limiting, meaning patients typically recover on their own within weeks to a couple of months. Unlike Hepatitis B or C, it does not progress to chronic liver disease.
Treatment of Hepatitis A
Currently, there is no specific antiviral medication for Hepatitis A. Treatment focuses on symptom relief and supportive care, such as drinking plenty of fluids, eating easily digestible foods, avoiding alcohol, and refraining from medications that may put extra strain on the liver. Most patients recover fully without long-term complications.
The most effective way to prevent Hepatitis A is vaccination, which provides long-lasting immunity. In addition, maintaining good hygiene practices—such as washing hands before meals and ensuring safe food and water consumption—are vital preventive measures.

Hepatitis B – Infection, Impact and Care
Hepatitis B Virus (HBV) is one of the most significant viral liver diseases, causing widespread health problems around the world. It is a major cause of cirrhosis and liver cancer, particularly in Southeast Asia, including Thailand. Hepatitis B infection can occur from birth through adulthood, and without proper prevention or treatment, it can lead to serious long-term health consequences.
Infection
Hepatitis B spreads primarily through contact with infected blood and bodily fluids. This includes unprotected sexual intercourse, sharing needles, unsafe tattooing or piercing practices, and mother-to-child transmission during childbirth. Infections that occur during infancy or early childhood—especially in newborns—have a much higher chance of developing into chronic infections compared to those acquired in adulthood.
Impact of Liver Diseases
Many people living with Hepatitis B show no symptoms in the early stages, making it difficult to know they are infected. However, the virus can silently cause chronic liver inflammation over time, leading to cirrhosis, liver failure, or liver cancer—conditions that are among the leading causes of death in Thailand. For this reason, individuals with chronic Hepatitis B should undergo regular monitoring and liver health check-ups.
Care and Management
While there is currently no cure that can completely eliminate Hepatitis B from the body, effective treatments can control the infection and reduce complications. Key approaches include:
- Hepatitis B vaccination: Highly effective in preventing infection, and part of the standard vaccination schedule for newborns in Thailand.
- Antiviral medications: For those with chronic infection and high risk of liver disease, antiviral drugs such as Tenofovir or Entecavir can suppress viral replication and slow disease progression.
- Liver-friendly lifestyle: Avoiding alcohol, maintaining a healthy diet, and getting regular medical check-ups are vital to protecting liver function.
Prevention
Prevention remains the most effective way to combat Hepatitis B, especially for high-risk groups such as healthcare workers, people with multiple sexual partners, and newborns. Early vaccination is the best defense and a crucial strategy to reduce the burden of this viral liver disease in the long term.
Hepatitis C – Risks, Chronic Symptoms and Modern Treatment
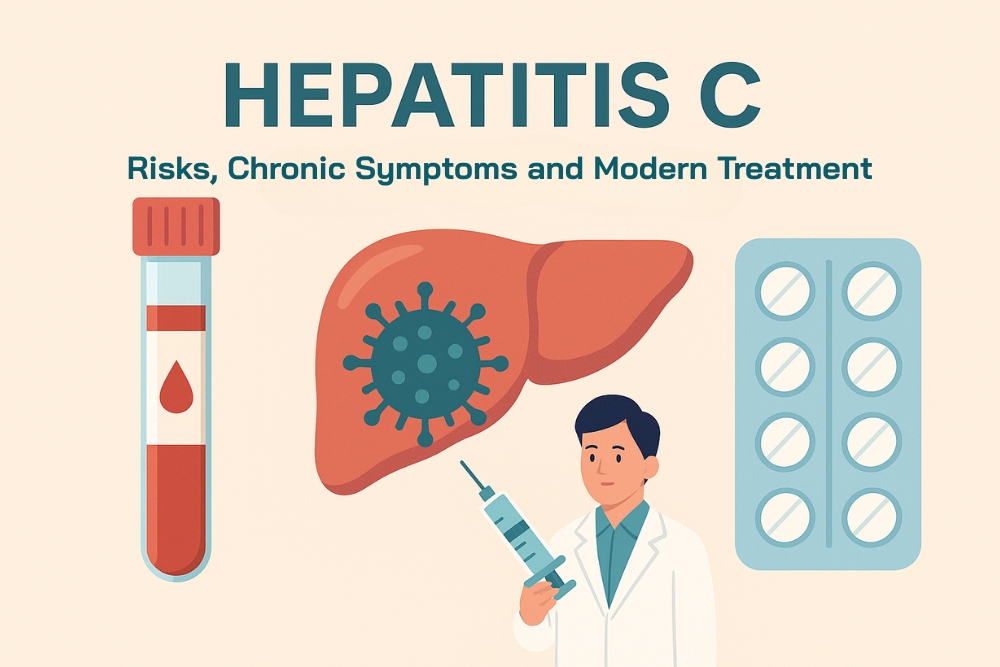
When it comes to Hepatitis C, many people may be less familiar with it compared to Hepatitis A or B. In reality, however, this disease is one of the silent threats that places a heavy burden on global public health and is a major cause of cirrhosis and liver cancer—two of the most serious liver diseases affecting many people in Thailand. What makes Hepatitis C particularly concerning is that there is still no available vaccine, making prevention and regular liver health check-ups absolutely essential.
Hidden Risks
Hepatitis C is primarily transmitted through blood-to-blood contact. Sharing needles, unsafe tattooing or piercing, and medical procedures performed with non-sterile equipment are major risk factors. In the past, transmission also occurred through unscreened blood transfusions or organ transplants. In addition, unprotected sexual activity—especially anal intercourse—can increase the risk of infection.
What makes this virus even more dangerous is that most people who are infected do not realize it, since the infection rarely shows noticeable symptoms in the early stages. As a result, it often progresses quietly until it becomes a chronic condition.
Liver Diseases and Chronic Symptoms That Often Appear Too Late
Unlike Hepatitis A, which resolves on its own, and Hepatitis B, which can be prevented through vaccination, Hepatitis C has a high likelihood of becoming chronic. It may take years—or even decades—before symptoms appear, by which time the liver may already be severely damaged. Signs of advanced disease include persistent fatigue, loss of appetite, weight loss, jaundice (yellowing of the skin and eyes), and abdominal swelling due to fluid retention. These are indicators of cirrhosis or severe liver disease.
Modern Treatments That Transform Lives
The good news is that modern medicine has revolutionized the treatment of Hepatitis C. A class of drugs known as Direct-Acting Antivirals (DAAs) has shown remarkable effectiveness, curing over 95% of patients within just 8–12 weeks. These medications have fewer side effects compared to older therapies like interferon, and many patients are now able to return to a normal quality of life.
This represents a major breakthrough: what was once considered a lifelong disease can now be completely cured with the right treatment. While Hepatitis C may seem distant, the reality is that it could be silently present in people around us without anyone knowing. Blood testing is the only way to confirm infection, and early detection dramatically improves the chances of successful treatment. The sooner patients access modern therapy, the lower their risk of developing cirrhosis and liver cancer in the future.
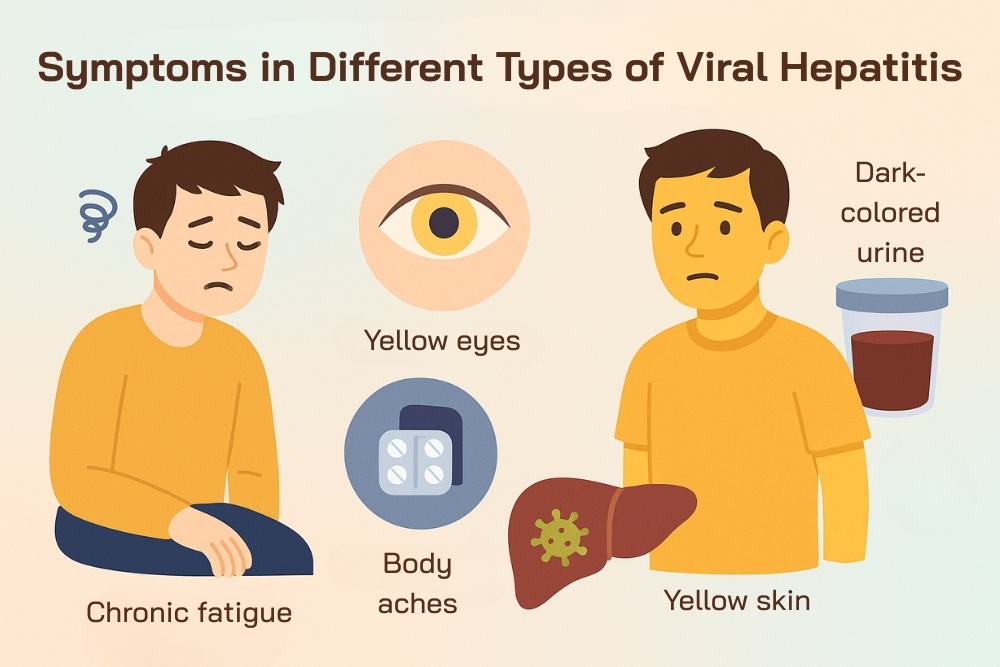
Symptoms to Watch for in Different Types of Viral Hepatitis
Viral hepatitis, whether type A, B, or C, often begins with non-specific symptoms such as fatigue, loss of appetite, or nausea. Many people mistake these signs for simple tiredness or common illnesses. However, ignoring these early warnings can allow the disease to progress into chronic inflammation, cirrhosis, or even liver cancer.
Key danger signs that suggest the liver may not be functioning properly include jaundice (yellowing of the skin and eyes), dark urine, pale stools, abdominal swelling, and persistent itching of the skin. Anyone experiencing these symptoms should seek medical evaluation promptly to detect and manage potential liver diseases in time.
| Aspect | Hepatitis A | Hepatitis B | Hepatitis C |
|---|---|---|---|
| Onset of Symptoms | 2–6 weeks after infection | 1–4 months after infection | Often no clear symptoms, may take years |
| Common Symptoms | Low-grade fever, fatigue, loss of appetite, nausea, abdominal pain | Fatigue, loss of appetite, nausea, joint pain, jaundice | Chronic fatigue, muscle aches, loss of appetite |
| Warning Signs | Jaundice, dark urine (usually resolves on its own) | Jaundice, dark urine (risk of chronic infection) | Jaundice, weight loss, abdominal swelling (often in advanced chronic disease) |
| Long-Term Risks | Does not cause chronic liver disease | Risk of cirrhosis and liver cancer if chronic | High risk of cirrhosis and liver cancer |
| Key Recommendations | Rest, drink plenty of fluids, vaccination available | Vaccination, regular testing, antiviral treatment if needed | Blood testing, modern antiviral drugs (DAAs) |
Complications of Viral Hepatitis: Cirrhosis and Liver Cancer
Viral hepatitis—particularly Hepatitis B (HBV) and Hepatitis C (HCV)—is a leading cause of serious liver diseases such as cirrhosis and liver cancer in Thailand. The major challenge is that many patients are unaware of their infection due to the absence of early symptoms. By the time they are diagnosed, the disease has often progressed significantly.
Cirrhosis
Cirrhosis occurs when healthy liver tissue is continuously damaged and replaced by scar tissue, reducing the liver’s ability to function. Patients may develop complications such as fluid accumulation in the abdomen (ascites), leg swelling, variceal bleeding in the esophagus, persistent skin itching, and hepatic encephalopathy (a form of brain dysfunction caused by liver failure). In Thailand, the most common causes of cirrhosis are chronic Hepatitis B and C, long-term alcohol use, and fatty liver disease.
Liver Cancer (Hepatocellular Carcinoma – HCC)
Liver cancer often develops in patients who already have cirrhosis. Continuous cycles of liver cell damage and repair can lead to mutations and cancer formation. Hepatitis B is particularly unique because it can integrate its genetic material into liver cells, increasing the risk of liver cancer even without cirrhosis.
Warning signs of liver cancer include unexplained weight loss, loss of appetite, persistent abdominal pain, abnormal abdominal enlargement, and prolonged jaundice.
Diagnosis of Viral Hepatitis
Diagnosis is the most critical step in managing viral hepatitis and other liver diseases, since many infected individuals show no symptoms in the early stages. Without timely testing, the disease may progress silently until it leads to serious complications such as cirrhosis or liver cancer. Appropriate diagnostic methods enable doctors to plan effective treatment and prevent further transmission.
Medical History and Physical Examination
The diagnostic process usually begins with a detailed medical history. Doctors will ask about risk behaviors, such as sharing needles, receiving tattoos or piercings in non-sterile settings, or having unprotected sex. They will also review vaccination history for Hepatitis B. A physical examination follows, checking for signs such as jaundice (yellowing of the skin and eyes) or an enlarged liver.
- Blood Tests
- Blood testing is the primary method of diagnosis, and several types are commonly used:
- Antibody test: Determines whether the patient has been previously exposed to the virus and whether protective immunity is present.
- Antigen and viral genetic material testing: For example, HBsAg for Hepatitis B or HCV RNA for Hepatitis C, which confirm active infection and ongoing viral replication.
- Liver function tests (LFTs): Measures enzymes such as ALT and AST to detect liver inflammation or damage.
- Additional Tests for Liver Assessment
- If infection is confirmed, further tests may be recommended to assess the extent of liver damage:
- Blood testing is the primary method of diagnosis, and several types are commonly used:
- Abdominal Ultrasound: Identifies abnormalities such as liver enlargement, cirrhosis, or tumors.
- FibroScan: A non-invasive method that measures liver stiffness to evaluate fibrosis and cirrhosis without the need for a biopsy.
- Liver Biopsy: In selected cases, a biopsy may be performed to provide a detailed evaluation of liver tissue damage.
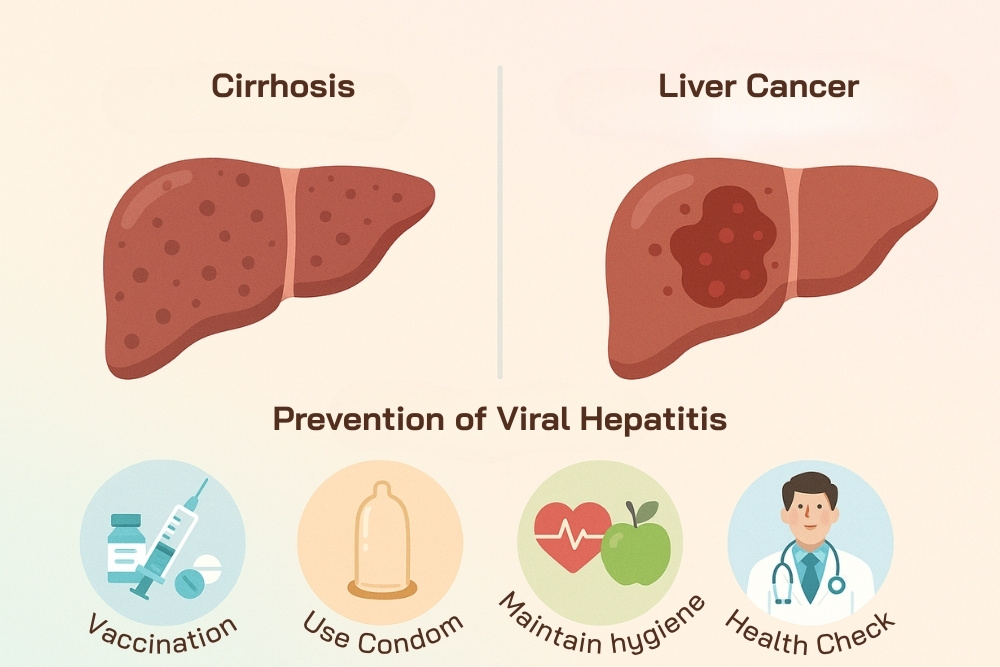
Vaccines and Prevention of Viral Hepatitis
Preventing viral hepatitis is far more effective than treating it, since once the infection enters the body—especially Hepatitis B and C—it may lead to chronic infection and serious complications such as cirrhosis or liver cancer. Vaccination, combined with healthy lifestyle practices, remains the most effective strategy to reduce the risk of developing these liver diseases.
Available Vaccines
- Hepatitis A: A highly effective vaccine that provides long-lasting immunity. It is recommended for individuals who have never been infected, particularly children, those living in high-prevalence areas, and travelers to regions where the virus is common.
- Hepatitis B: One of the core vaccines given to all newborns in Thailand at birth, with additional booster shots available for adults who were never vaccinated or lack immunity. This is the most effective measure to prevent chronic infection and liver cancer caused by HBV.
- Hepatitis C: Currently, there is no vaccine available due to the virus’s high mutation rate. However, major medical advancements have introduced new antiviral drugs that can cure Hepatitis C in most patients.
Prevention Beyond Vaccination
While vaccines significantly reduce the risk of infection, lifestyle and behavioral practices also play a critical role in protecting against viral hepatitis and related liver diseases. Key preventive measures include:
- Personal hygiene: Wash hands frequently, eat properly cooked food, and drink clean, treated water to reduce the risk of Hepatitis A.
- Avoid contact with blood or bodily fluids: Always use condoms during sexual intercourse and avoid sharing needles or any equipment that may be contaminated with blood.
- Safe medical and cosmetic procedures: For activities such as tattooing, body piercing, or dental treatments, always choose clinics or facilities that meet safety standards and use sterile equipment.
- Regular health check-ups and screening for high-risk groups: Individuals with risk behaviors or a family history of hepatitis should undergo routine blood tests to ensure early detection and treatment.
Together, vaccination and healthy lifestyle practices act as the best shield against viral hepatitis and serious liver diseases. The earlier one receives vaccines and adopts protective behaviors, the greater the chance of preventing dangerous long-term complications.
Related Article
VCT Day 2025 – Get Tested, Get Empowered
Conclusion: Why Early Screening and Prevention Matter for Liver Diseases
Hepatitis A, B, and C differ in transmission, severity, and treatment. Yet, they share one reality: without diagnosis or care, all can cause cirrhosis or liver cancer. These are among the deadliest liver diseases in Thailand. Early screening detects silent infections before symptoms appear. This makes timely treatment possible.
For Hepatitis C, modern antiviral therapies now provide a cure. In Hepatitis B and A, early vaccination remains the strongest shield against infection.
“Prevention also means making lifestyle changes: eating safe and hygienic food, drinking clean water, avoiding the sharing of needles or contaminated equipment, practicing safe sex with condoms, and undergoing regular health check-ups. When these habits are combined with vaccination and proper liver care, the long-term burden of viral hepatitis can be greatly reduced.”
Ultimately, early detection and prevention of viral hepatitis are about protecting yourself and others. They also safeguard your family and society from preventable, controllable diseases. With awareness and proactive care, a future free from viral hepatitis and serious liver diseases is within reach.
Reference:
รพ.จุฬาภรณ์แนะกลุ่มเสี่ยงเกิดก่อนปี 2535 ตรวจคัดกรอง-ฉีดวัคซีนป้องกันไวรัสตับอักเสบบี
https://www.hfocus.org/content/2025/08/34941
สาเหตุ “ตับอักเสบ” คนไทยกว่า 3 ล้านคน เสี่ยงติดเชื้อไวรัสตับอักเสบบีเรื้อรัง
https://www.pptvhd36.com/health/care/7367
จุฬาฯ เผยผลสำเร็จ 30 ปีแห่งการขจัดไวรัสตับอักเสบบีและซี